Introduction
The field of pharmaceutical regulatory affairs has played a critical role in ensuring that medicinal products are safe, effective, and of high quality. Over the last century, the need for a robust regulatory system has become increasingly evident due to historical drug tragedies and the rapid advancement of pharmaceutical sciences. The evolution of drug regulation has been shaped by public health emergencies, scientific innovation, and global cooperation. This article explores the historical development of drug regulations and how pharmaceutical regulatory affairs have evolved into a specialized, strategic discipline within the healthcare industry.
In the vast and intricate world of medicine, ensuring the safety, efficacy, and quality of pharmaceutical products is of paramount importance. Over the past century, the pharmaceutical industry has witnessed unprecedented growth, driven by advances in biomedical research, biotechnology, and global health demands. However, alongside this rapid innovation comes the critical responsibility of regulating drug development, manufacturing, marketing, and post-marketing activities. This is where pharmaceutical regulatory affairs play a vital role.
Regulatory affairs (RA) is a specialized function within the pharmaceutical, biotechnology, and medical device industries. It acts as the liaison between industry and government, ensuring that all products comply with regulatory requirements and legal obligations set by various national and international authorities. Regulatory professionals are involved throughout the entire drug lifecycle: from clinical trials and product registration to pharmacovigilance and label updates.
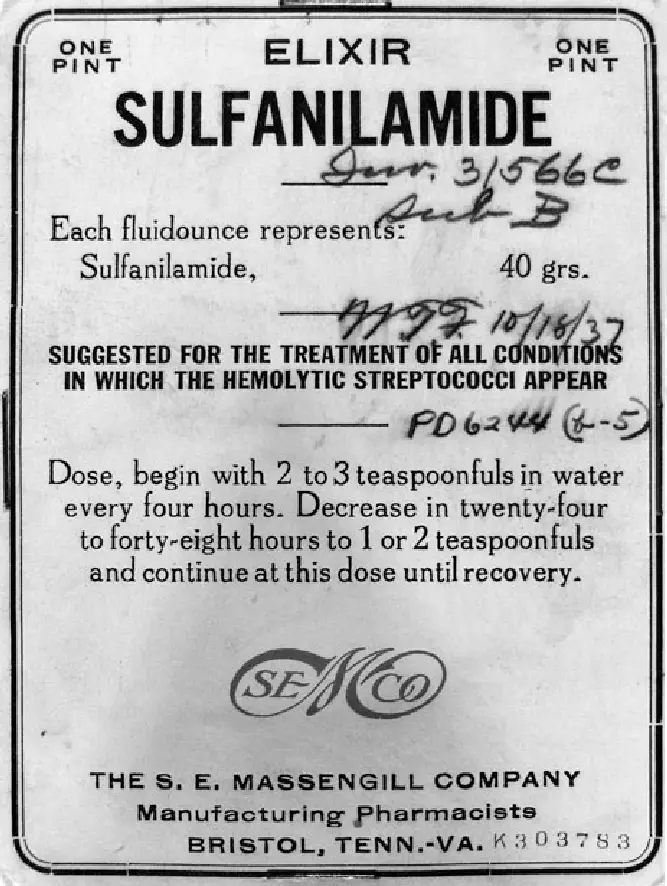
The modern regulatory landscape we know today is the result of decades of evolution, often driven by public health crises, such as the thalidomide tragedy of the 1960s or the Elixir Sulfanilamide disaster of the 1930s. These catastrophic events exposed the dangers of inadequate oversight and led to the development of stricter laws, regulatory bodies like the U.S. FDA, and frameworks such as the Kefauver-Harris Amendments, ICH guidelines, and the Common Technical Document (CTD) format.
In this article, we explore the historical trajectory of drug regulation, from its humble beginnings to its current strategic role in global health governance. We’ll also trace the evolution of pharmaceutical regulatory affairs as a career and functional domain, highlighting key legislative milestones, global harmonization efforts, and the future trends shaping the profession in the 21st century.
By understanding the past, we better appreciate the systems now in place to protect millions of lives worldwide through safe, effective, and high-quality medicines.
Early Beginnings: The Foundation of Drug Regulation
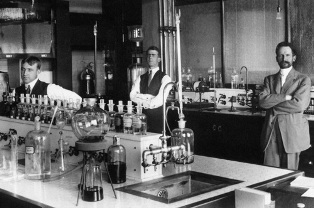
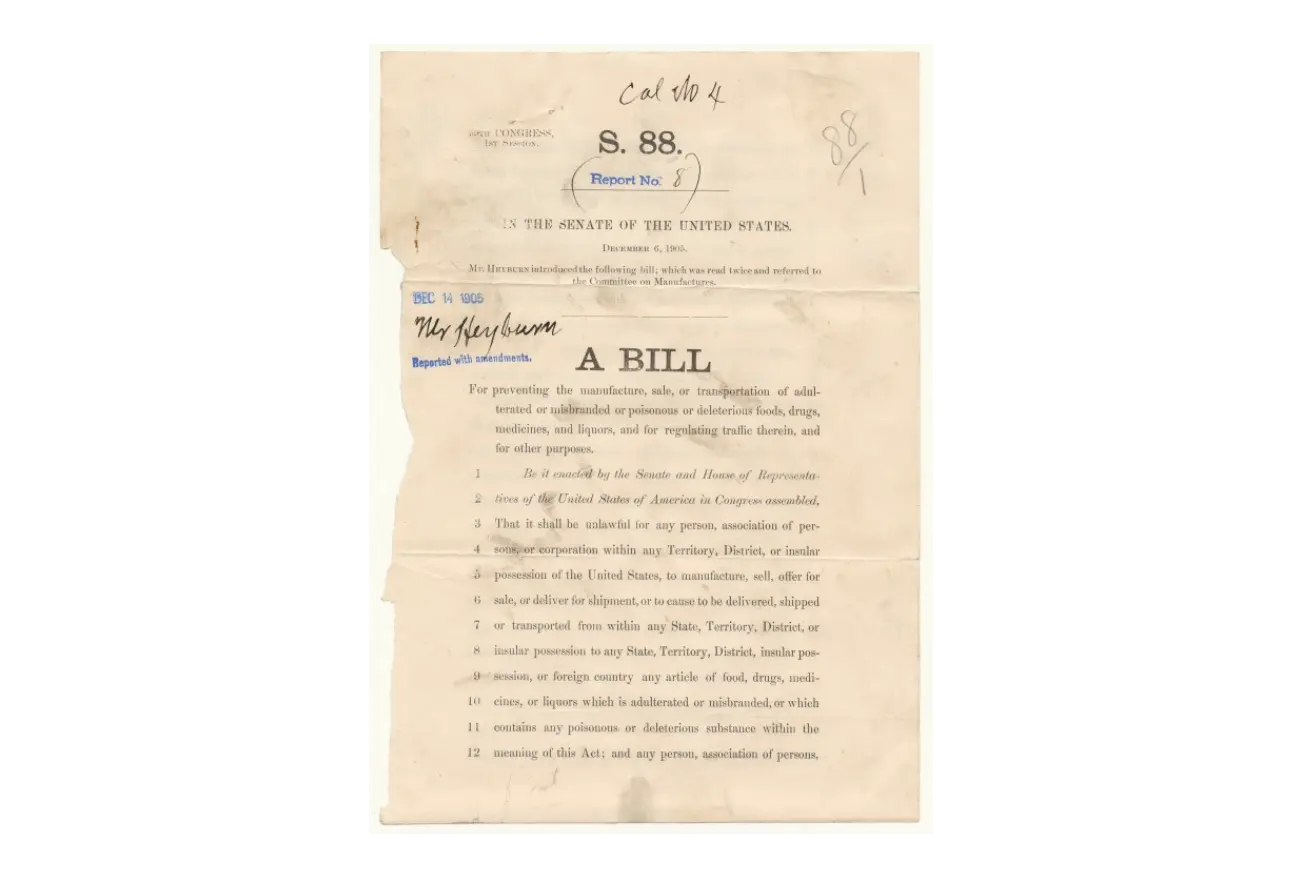
The earliest form of drug regulation in the modern era began in the United States with the Pure Food and Drug Act of 1906. Sparked by public outcry over dangerous and mislabeled medicines, the act aimed to prevent the manufacture and sale of adulterated or misbranded food and drugs. It marked the first major attempt to regulate the pharmaceutical market and laid the groundwork for the Food and Drug Administration (FDA).
However, this law lacked the enforcement strength and clarity needed to prevent harm effectively. It wasn’t until a major tragedy occurred in the 1930s that more rigorous regulations were put in place.
Pure Food and Drug Act of 1906
(Also known as the Wiley Act)
The Pure Food and Drug Act of 1906 was the first major U.S. federal law aimed at regulating the safety, labeling, and integrity of food and drugs. Signed into law by President Theodore Roosevelt on June 30, 1906, this Act marked the beginning of government-led consumer protection in the United States and laid the foundation for the creation of the U.S. Food and Drug Administration (FDA).
Historical Context
In the early 20th century, American markets were flooded with adulterated foods, misbranded medicines, and patent remedies that made unverified claims. Public pressure mounted after investigative journalism—especially Upton Sinclair’s novel The Jungle—exposed unsanitary practices in the meatpacking industry. Additionally, so-called “medicines” at the time often contained dangerous or addictive substances such as morphine, cocaine, alcohol, and opium, with no disclosure to consumers
Key Provisions of the 1906 Act
| Provision | Description |
| Misbranding Prohibition | Banned false or misleading labeling of food and drug products. |
| Adulteration Ban | Prohibited the sale of products that were tainted, spoiled, or contained harmful ingredients. |
| Label Transparency | Required the listing of certain dangerous substances (e.g., alcohol, morphine, cannabis, opium) on drug labels. |
| Interstate Commerce Regulation | Applied only to products shipped across state lines (limiting its scope). |
| Enforcement Agency | Enforced by the Bureau of Chemistry, which later became the FDA in 1930. |
Limitations of the 1906 Act
- While groundbreaking, the Act had significant limitations: it did not require pre-market safety testing for drugs.
- No authority to ban unsafe drugs—only to prosecute mislabeling or adulteration after harm occurred.
- No requirement for efficacy or scientifically supported claims
These gaps became evident in cases like the Sulfanilamide disaster (1937), ultimately leading to the Federal Food, Drug, and Cosmetic Act (1938), which replaced and expanded the 1906 Act.
Impact and Legacy
The Pure Food and Drug Act of 1906:
- Established the first federal standards for labeling and safety in the U.S. drug and food industries.
- Paved the way for modern drug regulation and the eventual formation of the FDA.
- Sparked further reforms in the 20th century, leading to stronger consumer protections.
Tragedy Sparks Change: The Sulfanilamide Disaster (1937)
In 1937, over 100 people—many of them children—died after consuming Elixir Sulfanilamide, which was formulated using diethylene glycol, a toxic chemical. This tragedy shocked the public and forced lawmakers to act swiftly. The result was the Federal Food, Drug, and Cosmetic (FD&C) Act of 1938, which required companies to prove drug safety before marketing them. This law also authorized factory inspections and increased the FDA’s enforcement powers. The 1938 Act was a monumental shift in drug regulation, as it formally introduced the concept of pre-market approval, setting a precedent that still exists today
Key Provisions of the FD&C Act (1938)
| Provision | Details |
| Pre-market Safety Approval | Drug manufacturers were now required to provide scientific evidence of a product’s safety before it could be marketed. |
| Labeling Requirements | Mandated accurate and complete labeling, including directions for use and warnings about potential dangers. |
| FDA Enforcement Authority | The FDA was granted power to inspect factories, seize unsafe products, and prosecute violators. |
| Cosmetic and Device Regulation | Extended federal oversight to include cosmetics and medical devices for the first time. |
| Court Injunctions | Allowed the FDA to take legal action to prevent the sale of misbranded or adulterated products. |
| Standardization of Definitions | Clarified the definitions of “drug”, “cosmetic”, “device”, “label”, and “misbranding” to enforce clearer compliance. |
Historical Impact
The FD&C Act laid the foundation for modern drug regulation. It marked a major shift from reactive measures to preventive regulation, ensuring that drug safety was assessed before products reached the public. Over time, it has been amended by critical legislation such as:
- Kefauver–Harris Amendments (1962) – Required proof of efficacy
- Orphan Drug Act (1983) – Incentivized rare disease treatment
- FDA Modernization Act (1997) – Streamlined regulatory processes
- 21st Century Cures Act (2016) – Promoted innovation and faster approval pathways
Advancing Oversight: Durham-Humphrey and Early Drug Monitoring
As the pharmaceutical industry grew in the 1940s and 1950s, further clarification was needed around drug distribution. The Durham-Humphrey Amendment of 1951 officially distinguished between prescription and over-the-counter (OTC) drugs. This was vital in controlling medication misuse and ensuring physician oversight for more potent therapies.
During this period, regulators also began to recognize the importance of adverse drug reaction (ADR) monitoring. However, systems were still rudimentary and underdeveloped—until another global drug disaster transformed regulatory philosophy.
Durham-Humphrey Amendment of 1951
(Prescription Drug Amendment)
The Durham-Humphrey Amendment, enacted in 1951, is a key amendment to the Federal Food, Drug, and Cosmetic (FD&C) Act of 1938. It was introduced by Senator Hubert H. Humphrey and Representative Carl Durham, and it established clear legal distinctions between prescription (legend) drugs and over-the-counter (OTC) medications.
This amendment addressed a growing concern: many drugs were potent enough to require medical supervision yet were still being sold without prescription requirements or proper usage guidance.
Key Provisions
| Provision | Description |
| Drug Classification | Legally divided medications into two categories: Prescription (legend) drugs and OTC drugs. |
| “Caution” Label Requirement | Required prescription drugs to carry the label: |
| “Caution: Federal law prohibits dispensing without a prescription.” | |
| Pharmacist Dispensing | Authorized licensed pharmacists to dispense prescription drugs only with a valid prescription from a licensed practitioner. |
| Verbal Prescriptions & Refills | Allowed verbal prescriptions (by phone) and refills of prescriptions if authorized by the prescribing physician. |
| FDA Authority | Empowered the FDA to determine which drugs must be dispensed by prescription only, based on their safety profiles and potential for misuse. |
By the late 1940s, more potent drugs—like antibiotics, barbiturates, and hormones—were widely available. These drugs could have serious side effects or require professional medical judgment for safe use. The 1938 FD&C Act lacked clear definitions about which drugs should be sold only with a prescription. The Durham-Humphrey Amendment filled this critical gap in regulatory policy.
Impact on Drug Regulation
- Created the modern prescription system still in use today.
- Reduced misuse of powerful medications.
- Ensured patients received medical oversight when taking certain drugs.
- Strengthened the role of pharmacists and enhanced patient safety through regulated dispensing.
Legacy
This amendment significantly influenced drug marketing, pharmacy practice, and FDA oversight. It also laid the groundwork for future regulations on controlled substances, prescription labeling, and drug advertising. Its influence continues in today’s distinction between prescription-only and non-prescription medicines globally.
The Thalidomide Crisis and the Kefauver-Harris Amendments (1962)
Perhaps the most defining moment in pharmaceutical regulatory history was the thalidomide tragedy of the late 1950s and early 1960s. Marketed in Europe and other countries as a treatment for morning sickness, thalidomide caused thousands of birth defects in babies born to women who took the drug during pregnancy.
In the U.S., thanks to FDA reviewer Dr. Frances Kelsey, thalidomide was never approved, preventing a similar catastrophe. Nonetheless, the global impact was profound and led to the landmark Kefauver-Harris Amendments of 1962 to the FD&C Act.
Key features of these amendments included:
- Mandatory proof of both safety and efficacy before marketing.
- Requirement for well-controlled clinical trials.
- Implementation of Good Manufacturing Practices (GMP).
- Informed consent from clinical trial participants.
- Greater FDA authority over advertising and labeling.
These changes transformed the drug approval process and shifted regulatory affairs from a reactive to a proactive discipline.
Kefauver-Harris Amendments of 1962
(Drug Efficacy Amendment)
The Kefauver-Harris Amendments, passed by the U.S. Congress in 1962, significantly strengthened the Federal Food, Drug, and Cosmetic Act (FD&C Act) of 1938. These amendments were named after Senator Estes Kefauver and Representative Oren Harris, and they fundamentally reformed the drug regulatory system in the United States.
They were introduced in response to the global thalidomide tragedy, which caused thousands of birth defects in Europe due to inadequate drug testing. The U.S. was largely spared, thanks to FDA officer Dr. Frances Kelsey, who refused to approve thalidomide without proper safety data.
Key Provisions
| Provision | Details |
| Proof of Efficacy Required | Drug manufacturers were now required to provide substantial evidence of effectiveness, in addition to safety, before marketing any drug. |
| Informed Consent | Required informed consent from all human participants in clinical trials. |
| GMP Regulations | Mandated Good Manufacturing Practices (GMP). |
| Adverse Event Reporting | Companies were required to report serious adverse drug reactions (ADRs) to the FDA. |
| Control of Drug Advertising | Transferred regulation of prescription drug advertising from the FTC to the FDA. |
| Preclinical and Clinical Trial Requirements | Introduced structured guidelines for preclinical testing and all phases of clinical trials (Phase I–IV) |
The thalidomide crisis revealed serious global shortcomings in drug regulation, particularly the lack of rigorous testing for efficacy and safety before approval. The Kefauver-Harris Amendments ensured that drugs were both safe to use and effective for their intended purpose, establishing a scientific basis for drug approval.
Impact on Modern Drug Regulation
- Established the requirement for randomized controlled trials (RCTs) to demonstrate efficacy.
- Strengthened the role of the FDA in reviewing drug applications and monitoring post-market safety.
- Created a scientific and ethical framework for drug development still used today.
- Marked the rise of evidence-based medicine in pharmaceutical regulation.
Legacy
The Kefauver-Harris Amendments are considered one of the most transformative reforms in U.S. pharmaceutical law. They enhanced public confidence in drug safety, formalized the drug approval process, and laid the groundwork for global regulatory standards that many countries later adopted or adapted.
Expansion and Globalization: 1970s–1990s
With rising international pharmaceutical trade and increasing complexity in drug development, the 1970s–90s saw further growth in regulation
Global Pharmacovigilance Systems
The World Health Organization (WHO) launched its international ADR monitoring program in 1968, leading to the establishment of the Uppsala Monitoring Centre in Sweden. Countries like the UK introduced the Yellow Card Scheme, which remains a cornerstone of post-market surveillance.
Orphan Drug Act (1983)
The U.S. also addressed the lack of incentives for developing drugs for rare diseases by passing the Orphan Drug Act. It provided tax credits, market exclusivity, and funding for companies developing treatments for diseases affecting small populations.
FDA Modernization Act (1997)
This act updated many drug approval processes, encouraged patient-centered reforms, and acknowledged the increasing importance of fast-track approvals and user fees for applications.
The Emergence of Regulatory Affairs as a Profession
Until the 1970s, regulatory activities were often carried out by scientists or legal experts within pharma companies. However, the growing complexity of regulatory frameworks gave rise to regulatory affairs (RA) as a dedicated career field.
Professionals in RA became responsible for:
- Preparing and submitting regulatory dossiers (INDs, NDAs, MAAs).
- Ensuring compliance with global regulations.
- Liaising with regulatory authorities.
- Monitoring post-approval obligations such as pharmacovigilance and labeling
With the global expansion of pharma, RA professionals increasingly require cross-border knowledge, communication skills, and familiarity with evolving regulations.
Ready to master the world of pharmaceutical regulatory affairs?
👉 Dive into our comprehensive guide and gain the knowledge you need to navigate regulations with confidence.
Harmonization and the Role of the ICH
To address discrepancies among regulatory requirements across regions, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) was established in 1990.
Its goals included:
- Harmonizing technical requirements across the U.S., EU, and Japan.
- Creating a standardized submission format: the Common Technical Document (CTD).
- Promoting global safety standards such as MedDRA (Medical Dictionary for Regulatory Activities).
ICH guidelines are now widely adopted across the globe, streamlining development and reducing duplication of effort in multinational submissions.
Regulatory Affairs in the 21st Century
Modern regulatory affairs professionals navigate an environment that is dynamic, global, and digitally driven. Key trends include
- Electronic submissions (eCTD)
- Real-world evidence (RWE) and post-marketing studies
- Integration of AI and machine learning in regulatory intelligence and pharmacovigilance
- Responding to emergency health needs, such as with COVID-19 vaccines via Emergency Use Authorizations (EUAs)
Electronic Submissions (eCTD)

The adoption of the Electronic Common Technical Document (eCTD) has transformed regulatory submissions globally. eCTD enables pharmaceutical companies to submit drug dossiers electronically in a standardized format, streamlining the review process for agencies such as the FDA, EMA, and PMDA. This digital transition reduces administrative burden, accelerates approval timelines, and improves regulatory compliance through enhanced document management and traceability.
Real-World Evidence (RWE) and Post-Marketing Studies
Regulatory agencies increasingly rely on Real-World Evidence (RWE) collected from sources like electronic health records, patient registries, and insurance claims to complement traditional clinical trial data. RWE is vital for ongoing post-marketing surveillance, assessing long-term drug safety, effectiveness, and expanding indications. Integrating RWE supports more informed regulatory decisions, especially for rare diseases and complex patient populations
Integration of AI and Machine Learning in Regulatory Intelligence and Pharmacovigilance
Artificial intelligence (AI) and machine learning are revolutionizing regulatory intelligence and pharmacovigilance by automating data analysis and signal detection. These technologies enable faster identification of adverse drug reactions, optimize safety monitoring workflows, and support predictive analytics for proactive risk management. Their integration enhances regulatory compliance and accelerates safety reporting in a data-intensive environment.
Responding to Emergency Health Needs: Emergency Use Authorizations (EUAs)
The COVID-19 pandemic underscored the critical role of Emergency Use Authorizations (EUAs) in expediting access to vaccines and therapies during public health crises. EUAs allow regulatory agencies to authorize the use of unapproved medical products based on preliminary evidence when no adequate alternatives exist. This approach balances urgency with ongoing safety monitoring, requiring continuous data submission post-authorization to ensure patient protection.
RA has evolved from a documentation role to a strategic function within companies—advising on drug development strategy, risk management, and regulatory pathways to accelerate access to medicines.
Conclusion
The journey of drug regulation and the evolution of pharmaceutical regulatory affairs represent a dynamic and ongoing commitment to safeguarding public health on a global scale. Historically, regulatory policies were largely reactive, implemented in response to tragedies such as the Elixir Sulfanilamide disaster and the thalidomide crisis, which exposed critical gaps in drug safety oversight. These events served as catalysts, driving governments and regulatory bodies to establish stricter drug approval processes, enhanced pharmacovigilance systems, and comprehensive good manufacturing practices (GMP).
Today, pharmaceutical regulatory affairs has transformed into a proactive and strategic discipline, integrating scientific innovation with legal compliance to facilitate the efficient development and market access of safe, effective, and high-quality medicines. This evolution is powered by international regulatory harmonization initiatives such as the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), which standardizes guidelines across major markets including the US, EU, and Japan.
As medical science rapidly advances, incorporating breakthroughs like biologics, gene therapies, and personalized medicine, the regulatory environment is adapting to meet the complex challenges of evaluating these novel therapies. Modern regulatory affairs professionals must navigate an increasingly complex landscape characterized by evolving regulatory frameworks, accelerated clinical trial designs, and innovative data sources such as real-world evidence (RWE) and artificial intelligence (AI)–driven safety monitoring.
Global collaboration remains a cornerstone of this evolution, with regulatory agencies working together to streamline approval processes and share safety data to ensure that patients worldwide have timely access to cutting-edge treatments. The future of pharmaceutical regulatory affairs will be shaped by continued advancements in digital health technologies, data transparency, and a growing emphasis on patient-centric approaches, reinforcing the ultimate goal: delivering innovative medicines while prioritizing patient safety and public health.
References
- Britannica. Pure Food and Drug Act (1906).
- FDA. Milestones in U.S. Food and Drug Law.
- FDA. 80 Years of the Federal Food, Drug, and Cosmetic Act.
- FDA. Part I: The 1906 Food and Drugs Act and Its Enforcement.
- U.S. Food and Drug Administration (FDA) — History
- Official FDA overview of the 1906 act and its impact on food and drug regulation:
- FDA – Milestones in U.S. Food and Drug Law
- (See “Pure Food and Drug Act of 1906” section)
- Encyclopedia Britannica
- Scholarly article explaining the Pure Food and Drug Act and its significance:
- Pure Food and Drug Act | History & Summary | Britannica
- National Library of Medicine.
The Pure Food and Drug Act: Consumer Protection - Britannica. Sulfanilamide Disaster.
- https://www.britannica.com/event/Elixir-sulfanilamide-disaster



This is a fascinating and crucial read. Understanding the history of pharmaceutical regulation is key to appreciating its vital role in public health today. Seeing how past tragedies shaped today’s robust frameworks provides invaluable context for all current and aspiring professionals in the field. A truly insightful piece