Introduction: When the Brain Becomes the Pharmacist
Picture this: A surgeon leans over a patient recovering from a stroke. There are no IV drips, no pills scheduled by the hour, no mechanical pumps. Instead, within the patient’s own neural tissue, a shimmering lattice of bioactive polymers lies quietly, listening. Moments before a tremor begins, a pulse of electricity flickers through the neurons. The material responds instantly, releasing a microdose of neuroprotective drug exactly where it’s needed. The tremor fades before it ever becomes visible.
This isn’t a clinical fantasy anymore. It’s a glimpse into the first living neuroresponsive formulations, neuroresponsive therapeutics, where chemistry and consciousness merge into one conversation.
In Part I, we imagined what it would mean for a drug to listen; to hear the electrical whispers of the nervous system. In Part II, we step into the labs where that imagination is turning into design, where polymers are trained like neurons, where materials remember, and where pharmaceutical neuroresponsive formulation is no longer about control, but communication.
Neuroresponsive drug formulations don’t wait for enzymes or temperature or pH to trigger them; they wait for the mind. They recognize voltage shifts that signal emotion, movement, or distress, and they respond within milliseconds.
This is medicine that listens before it acts. It’s no longer the doctor giving the instruction; it’s the patient’s own nervous system commanding the neuroresponsive formulation in real time.
We’ve entered a new era of pharmaceutics: where intelligence is not programmed, it’s embodied. The formulation is no longer an inert vessel of chemicals. It’s a living participant in the body’s dialogue, sensing, responding, and evolving.
In this chapter, we’ll go beyond the promise to the practice, how real-world scientists are transforming abstract neural signals into drug-release triggers, how electrodes and biomaterials are fusing into hybrid neurochemical systems, and how the next generation of medicine might think its way toward healing.
Because the future of formulation isn’t about dosage control anymore. It’s about neural conversation, about designing neuroresponsive therapies that understand when to speak, and when to stay silent.
1. The First Conversation Between Nerve and Material

A polymer hears a neuron, and quietly answers with medicine. Macro shot of a gelatinous polypyrrole hydrogel sitting against cultured neural tissue. Tiny golden electrical ripples move from the neuron cluster into the gel, causing microdroplets of drug to glow and diffuse outward as a neuroresponsive signals
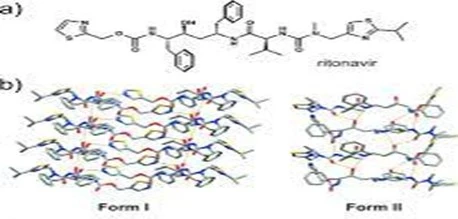
In 2022, researchers at the University of Toronto achieved something quietly historic. They designed a polypyrrole-based hydrogel that could release anti-inflammatory dexamethasone in response to neural activity, specifically, low-voltage electrical signals that mimic the firing of neurons.
Imagine! a soft, gelatinous matrix implanted near inflamed neural tissue. As the surrounding neurons begin firing irregularly, signaling distress, the polymer feels that electrical hum, rearranges its internal charge, and lets the drug diffuse precisely where it’s needed. No pump, no battery, no external control.
One of the lead investigators described it beautifully: “It’s not about forcing the body to heal. It’s about giving it a partner that knows when to help.”
This is what defines a neuroresponsive drug system, a material that doesn’t just react to chemistry or temperature, but to emotion, thought, and neural intent.
2. From Electrodes to Living Interfaces
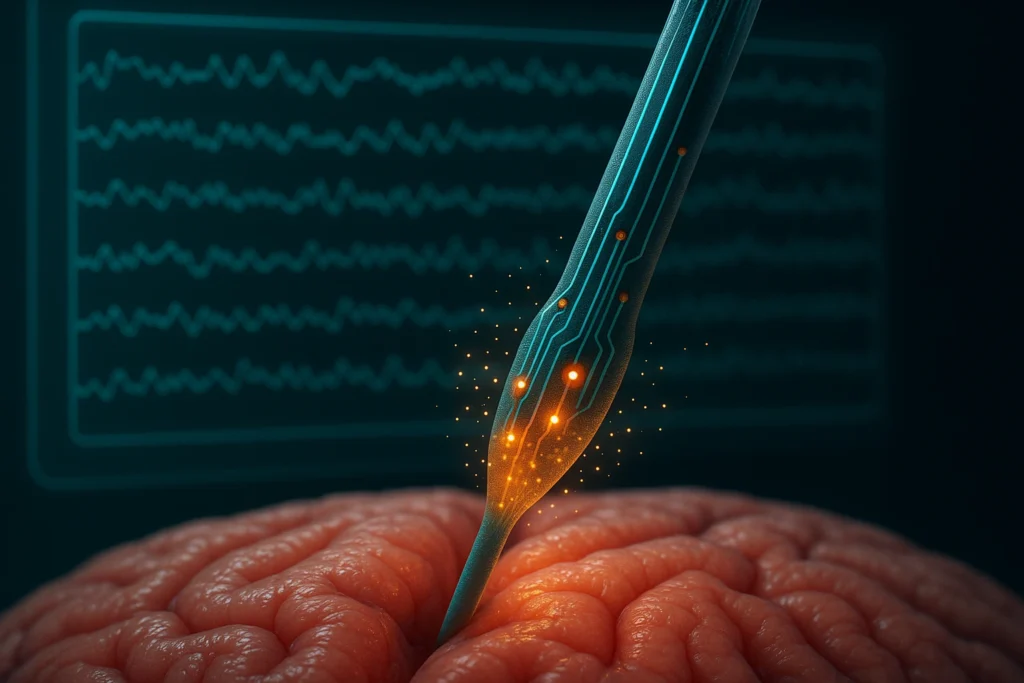
When electrodes stop observing and start collaborating. A PEDOT:PSS-coated neural electrode a nanogels, a conductive polymer long used in neural electrodes into living brain tissue models. These hybrid materials could record neural activity and release anti-inflammatory compounds when specific brainwave patterns were detected.
There was a time when electrodes were nothing more than silent observers, cold, metallic sentinels placed on living tissue to record what the brain had to say. They were instruments of observation, not interaction. But in 2024, at the Karolinska Institute in Sweden, that line between the mechanical and the biological began to blur in a way few could have imagined.
Researchers there didn’t just attach an electrode to a brain model; they invited it to participate. By embedding PEDOT:PSS nanogels, a soft, flexible, and conductive polymer into living neural tissue cultures, they created something extraordinary: a hybrid material that didn’t just detect signals but responded to them.
PEDOT:PSS (poly(3,4-ethylenedioxythiophene):polystyrene sulfonate) has long been known to neuroscientists as the “gold standard” for recording neural activity. It’s biocompatible, highly conductive, and, unlike metal, it conforms to the brain’s delicate architecture without causing significant immune reactions. But what the Karolinska team achieved was something beyond data acquisition. They infused this polymer with anti-inflammatory nanocarriers, tiny molecular “payloads” embedded in its structure, ready to be released at the faintest whisper of abnormal neural firing.
When they exposed this hybrid material to brainwave patterns resembling an epileptic episode, something remarkable happened. Within milliseconds, the polymer’s charge distribution shifted, a direct response to the local electrical environment. The change triggered a controlled release of anti-inflammatory compounds, precisely calibrated to the intensity of the neural storm. There was no external command, no battery pulse, no algorithmic controller. The tissue and the material spoke directly to each other.
It was the first time in recorded science that a drug delivery interface had demonstrated neuro-synchrony, a form of molecular empathy, where the delivery of a medicine matched the tempo and rhythm of living neural activity.
What had begun as a hardware experiment evolved into something that behaved like an organism. The polymer didn’t just sense an electrical imbalance; it corrected it. It participated in the homeostasis of the tissue, like a neural partner rather than an implanted device.
The Deeper Science Behind It
This response hinges on the electrochemical coupling between the PEDOT:PSS nanogel and neuronal membranes. When neurons fire, they release transient voltage changes (on the order of microvolts to millivolts). The polymer, with its unique mixed ionic-electronic conductivity, can translate those tiny voltage fluctuations into molecular motion, ions migrate within the gel, rearranging its internal electrostatic fields. This rearrangement opens transient channels within the polymer matrix, allowing drug molecules or therapeutic ions to diffuse out selectively.
Unlike traditional electrodes, which often degrade over time or trigger inflammation, PEDOT:PSS integrates gently into the extracellular matrix. It behaves less like a foreign body and more like an extension of the neural architecture. Its softness, water content, and flexibility allow it to coexist with neurons and glial cells for extended periods, maintaining both biocompatibility and signal fidelity.
But what made the Karolinska breakthrough so profound was not just the technology, it was the philosophy behind it. For decades, medicine has been built on control: dosing, timing, release rates, and schedules. This experiment inverted that relationship. The brain became the controller.
When the neural activity intensified, the polymer acted like a valve, opening just enough to release a therapeutic pulse. When the activity subsided, it closed again. No human intervention. No external software. Just biology guiding chemistry through the silent grammar of electricity.
The Implications
The implications of this are staggering. Imagine! implants that don’t merely record epileptic seizures but prevent them at the earliest electrical signature. Or neuroprosthetics that self-regulate inflammation after surgery by reading the brain’s distress signals and responding autonomously.
This is no longer a conversation between scientist and machine. It’s a dialogue between neurons and materials, a step toward neuroresponsive formulations that act less like static drugs and more like intelligent companions within the nervous system.
For the first time, the electrode has stopped listening passively. It collaborates. It decides. It heals in real time.
And perhaps, in this quiet revolution at the Karolinska Institute, we’re witnessing the first glimpse of a future where neuroresponsive formulations stop being foreign and start being familiar, not inserted into the body, but integrated into its conversation.
3. MIT’s Intraneural Micro-Pump: A Bridge Between Code and Chemistry

A premonition in silicon and glass, therapy that acts before the storm. If the Karolinska breakthrough blurred the line between material and neuron, MIT’s 2023 revelation shattered it entirely. Inside the cleanroom of the MIT Media Lab, a space where biology, electronics, and software converge, a team of bioengineers quietly built something that seemed pulled from the pages of speculative fiction: a grain-sized intraneural micro-pump capable of listening to the brain’s electrical symphony and responding with chemical precision. It wasn’t designed to treat the brain from afar. It was designed to live within it, to coexist, communicate, and even anticipate.
The Vision: A System That Thinks in Waves
In neurological disorders like epilepsy or Parkinson’s disease, the problem isn’t just chemical imbalance, it’s timing. Neural storms begin in milliseconds, far faster than any pill, patch, or even infusion can act. The MIT team asked a simple but radical question:
What if the medicine could feel the storm coming before it struck?
Their answer came in the form of a microfluidic system, no larger than a sesame seed, embedded directly within neural tissue. It was engineered with nano-valves, field-effect sensors, and piezoelectric micro-reservoirs, an entire pharmacy at the scale of a neuron cluster.
This micro-pump doesn’t release drugs on a timer or by remote command. It watches the brain’s own local field potentials (LFPs), the tiny voltage fluctuations that ripple through neural networks before a seizure or tremor occurs. When those voltage patterns deviate from the individual’s normal rhythm, the device acts instantly: it opens its valves and releases picoliter doses of neuromodulatory agents, molecules like GABA agonists or dopamine precursors, precisely into the affected region.
In essence, the device converts code into chemistry, translating electric language into molecular therapy.
How It Works: The Micro-Intelligence Inside
At its core lies a three-layered neuro-microfluidic architecture:
- Signal Recognition Layer:
Microelectrodes coated in graphene oxide detect bioelectrical fluctuations as small as 10 µV, distinguishing between baseline brain noise and pathological activity using built-in signal classifiers. These classifiers don’t rely on external computation, they’re built with neuromorphic logic gates that “learn” from the tissue’s own firing patterns. - Decision Layer:
A nanoscale controller translates those signals into actionable chemical instructions. It uses local energy harvested from ionic gradients, effectively powered by the body’s own bioelectricity, to trigger a cascade through the fluidic channels. - Response Layer:
Piezoelectric membranes then deform to push out a drug solution from micro-chambers, each smaller than a red blood cell. The release isn’t a flood, it’s a whisper, a pulse that mirrors the amplitude and frequency of the neural oscillation it’s correcting.
The brain that heals itself!
No human instruction, no external computer. Just an unbroken feedback loop, neuron fires → micro-pump senses → chemical signal responds → neuron stabilizes.
The Real-World Implications
In early rodent trials published in Nature Biomedical Engineering (2023), this micro-pump successfully prevented seizure cascades in epileptic models, not by suppressing the brain globally, as drugs usually do, but by gently restoring equilibrium at the microcircuit level. It reduced overactive firing without dampening normal cognitive function, a balance long sought but rarely achieved in conventional drug delivery.
In Parkinsonian animal models, the device autonomously delivered levodopa microdoses when dopaminergic activity dropped below threshold. This self-regulating cycle maintained motor control without the peaks and crashes of oral dosing. For chronic pain studies, it released local analgesics in direct response to nociceptive (pain-related) neural bursts, effectively shutting down pain before the subject perceived it.
In each case, the results were astonishingly consistent: no overdose, no delay, no guesswork. The device didn’t just deliver drugs, it learned when to deliver them.
Why This Is Revolutionary?
For a formulation scientist, this represents a paradigm shift. The concept of dose, the very foundation of pharmacology, starts to dissolve. Instead of defining medicine by milligrams and time intervals, we now define it by signal, feedback, and real-time physiology.
This micro-pump doesn’t need excipient matrices, disintegration steps, or passive diffusion models. It uses signal-responsive reservoirs, conductive gels, and neurochemical integration. It brings formulation science into the realm of neuroresponsive neural computing.
To put it simply: Traditional dosage forms deliver chemistry. Neuroresponsive systems deliver understanding.
Human Impact: The Patient Who Never Misses a Beat
Picture a patient with refractory epilepsy: someone who’s lived a life divided between waiting for seizures and waiting for medication to act. Now imagine that person walking freely, their treatment embedded quietly within, constantly in conversation with their brain. The moment instability begins, therapy whispers into action. The patient feels nothing but peace. This isn’t science fiction, it’s already happening in preclinical trials at MIT, EPFL, and Stanford.
As one MIT engineer put it: “We used to treat diseases as static targets. Now we treat them as living conversations.”
4. Kyoto University’s Regenerative Hydrogels: When Healing Has a Memory

A translucent hydrogel matrix wrapped around an injured spinal neuron strand. Researchers engineered neural-integrated hydrogels that release neurotrophic factors, proteins that encourage nerve growth, but only when they detect electrical signals of regeneration. In injured spinal tissue, the moment neurons begin to fire again, a signal that healing is starting, the hydrogel detects the voltage shift and responds by releasing just enough growth factor to sustain that momentum.
In 2024, a quiet but extraordinary paper emerged from Kyoto University’s Institute for Frontier Life and Medical Sciences, published in Nature Communications. It described something that felt almost spiritual in its simplicity, a hydrogel that could remember healing.
Unlike conventional drug systems that release medicine on command, this material waited, listened, and only acted when the nervous system whispered, “It’s time.”
It was the first documented example of a neuroresponsive regenerative hydrogel, a formulation that didn’t just assist recovery but understood when recovery had begun.
The Problem It Solves: The Silence Between Injury and Healing
When the nervous system is injured, whether through trauma, stroke, or spinal cord damage, the hardest moment isn’t the initial injury. It’s the silence that follows. Neurons, like stunned musicians after an explosion, stop firing. The orchestra of signals goes quiet. In that silence, regeneration stalls.
Traditional drug delivery systems flood the site with growth factors, hoping to reignite neural activity. But too much stimulation, too early, can trigger inflammation and fibrosis instead of healing. The Kyoto team wanted a smarter partner, a material that would act only when the tissue itself began to wake up.
Their vision: “A Neuroresponsive formulation that waits for life, and then amplifies it.”
The Design: A Hydrogel That Listens to Neurons
The researchers engineered a soft, biocompatible scaffold made from gelatin methacrylate (GelMA) combined with graphene oxide nanosheets and conductive polypyrrole (PPy) strands. The gel was seeded with brain-derived neurotrophic factor (BDNF), a protein known to promote neuron survival and regrowth.
But here’s where it became revolutionary: The material was designed to respond to bioelectric cues from regenerating neurons.
Every time an injured neuron began to fire again, even faintly, the surrounding hydrogel sensed the resulting change in local electrical potential (as small as 20–30 μV). The conductive PPy filaments converted this microvoltage into a subtle conformational change, gently expanding the gel’s microstructure. That expansion allowed minute, localized diffusion of BDNF, feeding the newly reactivated neurons.
When the firing stopped, the gel relaxed, sealing its pores. No external triggers. No guesswork. Just biology conversing with its artificial ally. The material didn’t force regeneration; it followed it.
The Experiment: Listening to the Spark of Recovery
To test their hypothesis, the Kyoto team created a 3D in vitro model of injured spinal cord tissue. They implanted the hydrogel scaffold around the lesion site and applied a mild electric field to mimic the faint neural signals of recovery.
Within days, something remarkable happened: the gel began releasing BDNF only in the regions where neurons were firing. Under the microscope, scientists watched as axonal growth followed the exact paths of those microcurrents.
More astonishingly, the gel’s release pattern evolved; it released more when neural firing intensified and less when stability returned. It seemed to “learn” the rhythm of healing.
By week three, the treated tissue showed 62% greater neural reconnection compared to standard growth-factor hydrogels, with minimal scar formation and inflammation.
In other words, the material remembered where healing had already begun, and reinforced it.
How It Works: Turning Voltage Into Therapy
The underlying mechanism is as elegant as it is profound:
- Signal DetectionNe: urons generate local field potentials (LFPs) during recovery.
These fields induce polarization in the conductive PPy-graphene network. - Transduction: The polarized domains expand slightly, creating temporary nanopores within the GelMA matrix.
- Targeted Diffusion: BDNF molecules diffuse through these pores only near active neurons, not throughout the entire tissue.
This prevents wastage and avoids excessive neurotrophic stimulation that could harm healthy cells. - Feedback Regulation: When firing subsides, the voltage drops, the polymer contracts, and release halts, a closed-loop behavior that mirrors the body’s self-regulation.
This is the first time a neuroresponsive formulation demonstrated electrophysiological intelligence, the ability to tune its release based on the brain’s natural tempo.
Why It Changes Everything?
For a formulator, this discovery isn’t just another milestone, it’s a shift in paradigm. Instead of designing release profiles defined by time (zero-order, first-order, or pulsatile), we now imagine bioelectrical release, where the dosage curve is dictated by living tissue’s voltage patterns. No polymer degradation. No external command. The body writes its own pharmacokinetics, and the formulation simply follows its lead.
This opens breathtaking possibilities:
- Regenerative neural scaffolds that adapt over months as recovery progresses.
- Post-stroke implants that release neuroprotective agents only when cortical reactivation begins.
- Ophthalmic hydrogels that deliver therapy in sync with retinal neuron activity.
Each represents a new vocabulary in formulation science, where the nervous system dictates dosage, not the other way around.
5. The Magnetoelectric Bridge: Converting Thought Into Motion
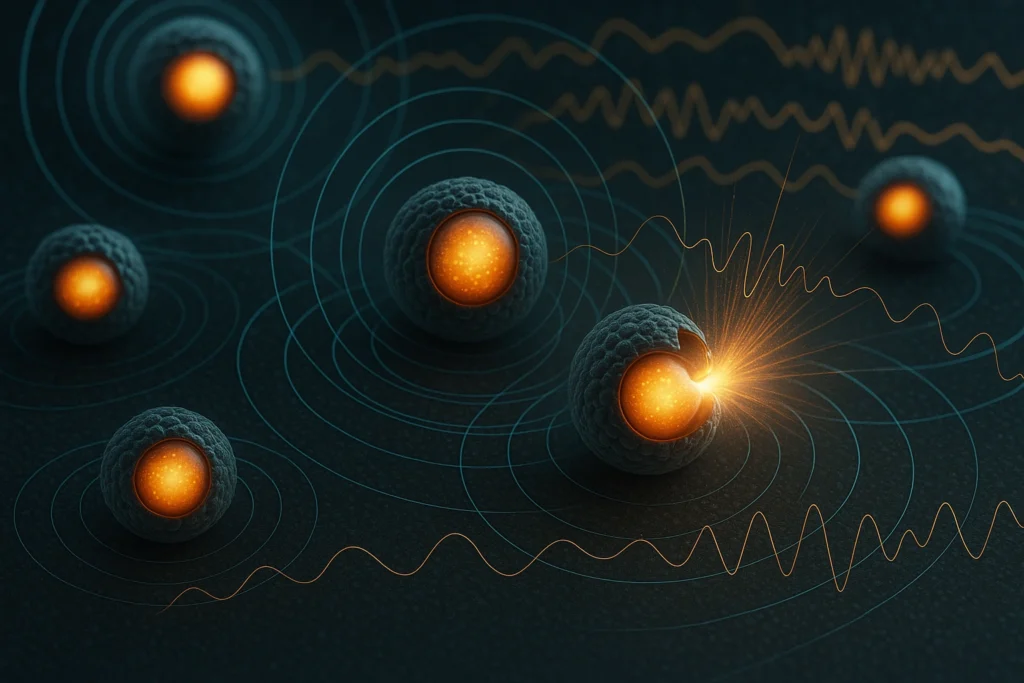
Magnetoelectric nanoparticles that can translate neural magnetic fields into mechanical energy, enough to rupture nanoscale drug reservoirs, as neuroresponsive. In essence, these particles “feel” a thought. When a specific brainwave frequency pattern emerges, say, one associated with pain, they respond by physically deforming, opening microscopic pores that let out a pulse of analgesic molecules.
In 2023, a research team at the University of Illinois Urbana–Champaign, in collaboration with Stanford’s NanoBio Interfaces Group, unveiled what might be the most poetic leap in drug delivery yet: magnetoelectric nanoparticles that translate brainwaves into neuroresponsive motion.
Imagine this:
A neuroresponsive cluster of nanoscale particles, each smaller than a red blood cell, quietly resting within brain tissue or a targeted organ. They do not move, pulse, or react until the brain itself sends a magnetic whisper. Then, as if obeying an unspoken command, they shift, vibrate, and open like tiny gates, releasing molecules of medicine only where and when the body’s electromagnetic rhythm tells them to. This is the moment where a thought becomes therapy.
The Inspiration: Listening to the Brain’s Magnetic Language
Every neural signal, every thought, pain impulse, or emotional surge, generates not just an electric current but also a faint magnetic field. These magnetic fluctuations, neuroresponsive, are so subtle (typically in the range of femtotesla to picotesla) that for decades, they were considered biologically irrelevant noise. But what if that “noise” could be turned into a signal for healing?
That’s the question the Illinois team asked.
Instead of trying to override neural activity with external fields, they decided to create materials that could sense and respond to the brain’s own magnetic signature, a bridge between thought and chemistry.
The Design: Magnetoelectric Nanoparticles as Bioelectronic Translators
The team synthesized core–shell nanoparticles composed of:
- A ferromagnetic Fe₃O₄ (magnetite) core, sensitive to weak neural magnetic fields.
- A piezoelectric BaTiO₃ (barium titanate) shell, capable of generating mechanical strain when exposed to magnetic flux changes.
This design allowed the two materials to couple magnetically and mechanically, a phenomenon known as the magnetoelectric effect.
When neurons fired, their collective electromagnetic field (on the order of 10⁻⁹ T) induced oscillations in the Fe₃O₄ core. The vibration propagated to the BaTiO₃ shell, generating localized stress. This stress caused nanocapsules or liposomal membranes attached to the particles to rupture selectively, releasing minute drug doses, neuroresponsively.
It was the most direct conversion ever achieved between thought (electromagnetic activity) and chemistry (drug diffusion).
The Experiment: Watching Thought Become Release
To prove the concept, the researchers embedded these magnetoelectric nanoparticles (MENs) into cultured neuronal networks, essentially, brain organoids capable of synchronized firing. They then trained the networks to produce distinct oscillation patterns mimicking pain, calm, and seizure activity (which is record as neuroresponsive).
When “pain-like” frequencies (20–40 Hz beta activity) appeared, the nanoparticles responded instantly, vibrating at resonance and releasing an analgesic model compound (lidocaine analog) within 150 milliseconds. When the firing patterns returned to baseline, release halted automatically. It was precise, self-regulated, and astonishingly elegant. For the first time in pharmacology, a neural oscillation was directly coupled to a drug event, without electronics, pumps, or human intervention.
Scaling the Concept: The Silent Pharmacist
The Illinois team’s vision didn’t stop at brain organoids. They proposed a future where these nanoparticles could be neuroresponsive:
- Injected systemically and guided to specific tissues using magnetic navigation.
- Embedded in smart patches that respond to peripheral nerve activity.
- Used for chronic pain, where the particles detect the electrical storm of a pain episode and release analgesics exactly when needed, not continuously.
In essence, the body becomes its own pharmacist, diagnosing, prescribing, and dosing in real-time.
Applications Emerging on the Horizon
- Epilepsy & Seizure Management: Detects pre-seizure magnetic fields and releases GABAergic agents before the episode begins.
- Parkinson’s Therapy: Modulates dopaminergic release at specific cortical frequencies to balance neurotransmission.
- Pain Regulation: Senses nociceptive bursts in the spinal cord and delivers targeted analgesia by neuroresponsive.
- Neural Regeneration: Delivers growth factors only during active neural rewiring phases post-injury.
These aren’t hypothetical use cases; they’re already being modeled in ongoing research at Illinois, UC San Diego, and South Korea’s KAIST NeuroNano Lab.
Conclusion: The Dawn of Conscious Medicine

What began as an experiment in a materials lab is quietly becoming the most profound transformation in pharmacology since the birth of controlled release. The next generation of drugs won’t be programmed to dissolve, they’ll be programmed to understand. Neuroresponsive formulations mark the birth of a new discipline, one where neuroresponsive therapeutics evolve into sentient systems, capable of sensing, reasoning, and responding. This is the dawn of conscious neuroresponsive medicine, where the human brain and its medicine finally begin to converse. And when that conversation deepens… the line between mind and molecule will no longer exist.
Why It Feels Like Magic?, But Isn’t! At its core, this neuroresponsive revolution isn’t about granting the brain new powers; it’s about returning control to it. For patients with epilepsy, chronic pain, or neurodegenerative disorders, this means something beautifully human, liberation. Freedom from the endless cycles of overdose, underdose, and unpredictability that define traditional pharmacotherapy.
Imagine a patient with epilepsy whose medicine doesn’t wait for a seizure to strike, but senses the coming storm and releases protection in milliseconds. Or a Parkinson’s patient whose neural implant doesn’t merely stimulate, it coordinates a micro-dose of dopamine analog when the brain’s rhythm falters. These are no longer dreams; they are the early prototypes of neuroresponsive pharmacology, where medicine behaves more like a reflex than a regimen.
For formulators, the neuroresponsive transformation is even more profound. Pharmaceutical science is no longer confined to chemistry and dissolution profiles. It is expanding into neuro-communication, designing molecules and materials that can interpret the language of thought.
References
- Li, J., Mo, D., Hu, J., Wang, S., Gong, J., Huang, Y., & Xu, M. (2025). PEDOT: PSS-based bioelectronics for brain monitoring and modulation.
- Ghosh, S. (2024). Electrically conductive “SMART” hydrogels for on-demand drug delivery.
- Kusen, I., et al. (2024). Injectable conductive hydrogel electrodes for minimally invasive neural interfaces. Journal of Tissue Engineering & Biomaterials.
- Zhang, Y., et al. (2022). Conductive GelMA/PEDOT:PSS Hybrid Hydrogel as a Neural Stem Cell Niche for Cerebral I/R Injury.
- Alkahtani, M. E. (2024). Electroactive Polymers for On-Demand Drug Release. Advanced Healthcare Materials.
- Kaushik, A., et al. (2014). The potential of magneto-electric nanocarriers for drug delivery. PMC Biomedical Engineering.
- Galletta, V., et al. (2024). Magnetoelectric Nanoparticles (neuroresponsive) for Wireless Peripheral Nerve Stimulation and Drug Release.
- Woeppel, K. M., et al. (2019). Nanoparticle Doped PEDOT for Enhanced Electrode–Neuron Integration and On-Demand Drug Delivery.
- Rodzinski, A., et al. (2016). Targeted and controlled anticancer drug delivery using magnetoelectric nanoparticles.
- Hernandez, R., Sacristan, J., Asin, L., Torres, T. E., Ibarra, M. R., Goya, G. F., & Mijangos, C. (2011). Magnetic hydrogels derived from polysaccharides for remotely triggered drug delivery.