What is an IND (Investigational New Drug)?
Introduction:
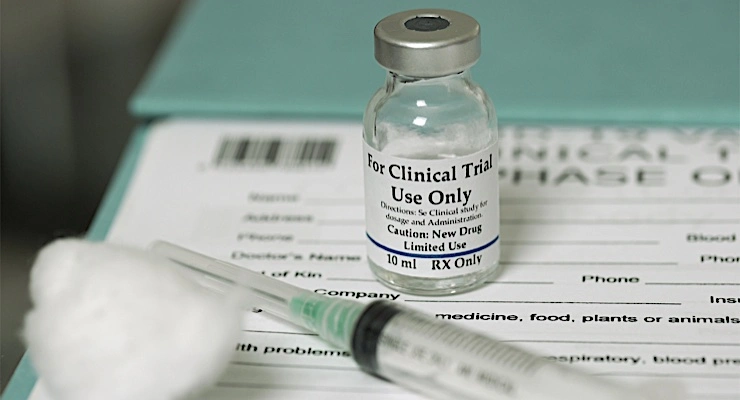
Investigational New Drug application is a critical regulatory submission filed with the U.S. Food and Drug Administration (FDA) to request authorization to begin clinical trials in humans. It serves as the bridge between pre-clinical research and human testing, ensuring that new drugs/pre-clinical drugs are reasonably safe for initial use in humans and that clinical trials are designed in a scientifically sound and ethical manner.
Without an approved new drug, no experimental drug may legally proceed to clinical testing in the United States.
This early-phase FDA submission includes detailed information on laboratory and animal testing, manufacturing methods, and a proposed clinical trial protocol. Its primary goal is to demonstrate that the experimental therapy meets safety standards and that the clinical trial is designed in a scientifically rigorous and ethically compliant manner.
Submitting a successful regulatory request to begin human trials is a critical milestone in the drug development process, serving as the gateway to further clinical evaluation and eventual FDA approval.
Purpose of a Test Drug/ Experimental drug/ Clinical phase drug:
The primary goal of a clinical-stage drug is to demonstrate its safety, efficacy, and therapeutic potential in humans through well-designed clinical trials. During this phase of drug development, researchers aim to confirm that the investigational treatment provides meaningful clinical benefits, has an acceptable safety profile, and meets the regulatory requirements necessary for eventual FDA approval.
- Protect human subjects involved in clinical trials with safety.
- Ensure the scientific quality and ethical standards of the proposed study.
- Allow the FDA to oversee new drugs before they are tested in humans.
Key Objectives of an Early phase drug Application
The key objectives of an early-phase drug application—such as an Investigational New Drug (IND) submission—are to ensure that the experimental therapy is safe for human testing, and that the proposed clinical trial design is both scientifically sound and ethically compliant. This critical stage in the drug development process aims to provide regulatory authorities, such as the FDA, with comprehensive preclinical data, including pharmacology, toxicology, and manufacturing information. The ultimate goal is to gain authorization to initiate Phase 1 clinical trials, marking the transition from laboratory research to first-in-human studies.
- Assess Safety for Human Testing
Based on animal studies and lab data (non-clinical safety). - Ensure Quality and Manufacturing Controls
Through Chemistry, Manufacturing, and Controls (CMC) documentation. - Evaluate Clinical Trial Design
Including protocols, endpoints, investigator qualifications, and informed consent.
Main Components of the new drug/ experimental drug
The main components of a new drug or experimental drug include its active pharmaceutical ingredient (API), excipients, formulation, and delivery mechanism. The active ingredient is the core substance responsible for the intended therapeutic effect, while excipients support the drug’s stability, absorption, and bioavailability. The formulation defines how the drug is prepared (e.g., tablet, injection, capsule), and the delivery system determines how the drug reaches its target site in the body. These components play a crucial role in the drug’s safety, efficacy, and overall performance during clinical trials and development. A thorough understanding of each element is essential for meeting regulatory requirements and advancing the drug through the FDA approval process.
- Preclinical (Animal) Study Data
- CMC (Chemistry, Manufacturing & Controls)
- Clinical Protocols for Proposed Human Studies
- Investigator Brochures and CVs
- IRB and Informed Consent Documentation
1. Pre-clinical (Animal) Study Data
Preclinical (animal) study data are a fundamental part of the drug development pipeline, providing essential information on the safety, toxicity, and pharmacological effects of a new or experimental compound before testing in humans. These studies use relevant animal models to evaluate how the candidate medicine is absorbed, distributed, metabolized, and eliminated by the body (ADME). The data helps identify safe dosage ranges and potential adverse effects, supporting regulatory submissions to agencies like the U.S. Food and Drug Administration (FDA). Comprehensive and reliable preclinical results are critical to progressing to the first stage of human clinical trials.

- Purpose: Demonstrates that the drug is reasonably safe for initial testing in humans.
- Includes:
- Pharmacology: How the drug affects the body (mechanism of action).
- Toxicology: Potential harmful effects (acute, sub-chronic, chronic toxicity).
- ADME studies: Absorption, Distribution, Metabolism, and Excretion
2. CMC (Chemistry, Manufacturing, and Controls)
Chemistry, Manufacturing, and Controls (CMC) refers to the comprehensive set of processes and documentation that ensure the consistent quality, purity, potency, and safety of a drug product throughout its development and production. CMC covers all aspects of the chemical composition, formulation development, manufacturing methods, and quality control testing necessary to produce a reliable and reproducible medication. Regulatory agencies such as the FDA require detailed CMC information as part of drug submissions to confirm that the product can be manufactured to meet stringent standards. Robust CMC data is crucial for advancing drug candidates through clinical trials and achieving final market approval.
- Purpose: Ensures consistent production of the drug with acceptable quality. Includes:
- Drug substance & drug product information
- Manufacturing process and controls
- Stability data
- Specifications and analytical methods
3. Clinical Protocols for Proposed Human Studies
Clinical protocols for proposed human studies are detailed, scientifically designed plans that outline the objectives, methodology, and procedures for conducting clinical trials involving new or experimental therapies. These protocols define critical elements such as study design, patient eligibility criteria, dosage regimens, safety monitoring, and endpoints to assess the drug’s efficacy and safety. Developing clear and thorough clinical protocols is essential to ensure that trials are conducted ethically, comply with regulatory standards, and generate reliable data for regulatory review by agencies like the FDA. Well-prepared protocols help minimize risks to participants while maximizing the potential to obtain meaningful clinical results.
- Purpose: Describes how human trials will be conducted.
- Includes:
- Study design (e.g., randomized, blinded, dose-escalation)
- Study objectives and endpoints
- Inclusion/exclusion criteria
- Monitoring and safety procedures
4. Investigator Brochures and CVs
Investigator brochures and curriculum vitae (CVs) are essential documents in the clinical trial process that support regulatory submissions and study oversight. The In
Brochure (IB) provides a comprehensive summary of all relevant preclinical and clinical data on therapy, including safety, pharmacology, and dosing information, helping clinical investigators understand the risks and benefits involved. Meanwhile, investigator CVs document the qualifications, experience, and credentials of the clinical trial investigators, demonstrating their ability to conduct the study ethically and competently. Together, these documents ensure compliance with FDA regulations and Good Clinical Practice (GCP) guidelines, facilitating a smooth and credible clinical trial process.
- Purpose: Provides background and qualifications of those conducting the clinical trials.
- Includes:
- Investigator’s Brochure (IB): Summary of clinical and nonclinical data, dosing info, side effects.
- Investigator CVs: Demonstrates qualifications and experience.
- Form FDA 1572: Statement of investigator’s commitment.
5. IRB (Institutional Review Board) and Informed Consent Documentation
The Institutional Review Board (IRB) plays a critical role in safeguarding the rights, safety, and well-being of human participants in clinical trials. The IRB is responsible for reviewing and approving study protocols to ensure they meet ethical standards and regulatory requirements before any research involving humans begins. Alongside this, informed consent documentation is a mandatory process that provides potential participants with clear, comprehensive information about the study’s purpose, procedures, risks, and benefits. This ensures participants voluntarily agree to join the trial with a full understanding of what participation entails. Together, IRB approval and properly executed informed consent forms are essential for ethical compliance, regulatory adherence, and building trust in clinical research.
- Purpose: Ensures ethical oversight and protection of human subjects.
- Includes:
- IRB Approval Letters: Documentation that the proposed clinical trial protocol has been reviewed and approved by an IRB.
- Informed Consent Forms (ICFs): Templates of the documents that will be provided to study participants explaining:
FDA Review Timeline for a clinical-stage drug:
- The FDA has 30 calendar days after receiving a test drug to review it.
- If no clinical hold is placed, the study can begin.
- If the experimental drug is incomplete or unsafe, the FDA may issue a clinical hold.
Global Equivalent Terms for Experimental Drug:
| Region | IND Equivalent |
| Europe (EMA) | IMPD (Investigational Medicinal Product Dossier) |
| Canada | CTA (Clinical Trial Application) |
| India | Clinical Trial Application (as per NDCT Rules) |
| Japan | Clinical Trial Notification (CTN) |
Why the early-phase trial drug matters

The early phase trial drug is the critical first step in bringing a new drug to market. Without FDA approval of this application, clinical trials cannot legally begin in the U.S. It ensures that only scientifically sound and ethically justified trials move forward. The experimental drug is essential to protect human health, meet regulatory standards, and launch a safe and successful clinical development program
- Ensures Safety Before Human Testing
- Meets FDA Legal Requirements
- Supports Ethical Conduct of Trials
- Establishes Scientific and Manufacturing Standards
- Lays the Foundation for Drug Approval
1. Protects Human Subjects Through Pre-clinical Safety Evaluation
Pre-clinical safety evaluation is a crucial step in the drug development process that protects human subjects by thoroughly assessing the potential risks of new therapies before they enter clinical trials. Through rigorous toxicology studies, pharmacology assessments, and animal testing, researchers identify any harmful effects, safe dosage ranges, and potential side effects of the experimental drug. This essential safety data helps regulatory agencies like the FDA ensure that only compounds with an acceptable risk profile proceed to human testing, minimizing harm and safeguarding participants in early-phase clinical trials
Primary Goal: Ensure this new drug is safe enough for initial use in humans.
- The new drug includes pharmacology and toxicology data from animal studies (preclinical testing).
- FDA scientists review this data to identify:
- Organ toxicity
- Safe starting doses for humans
- Potential side effects
Without this step, human participants could be exposed to unacceptable risks
2. Meets Legal and Regulatory Requirement
Ensuring that a drug development program meets legal and regulatory requirements is fundamental to gaining approval from health authorities such as the U.S. Food and Drug Administration (FDA) and other global regulatory agencies. Compliance involves adhering to strict guidelines covering clinical trial design, safety monitoring, manufacturing practices, and documentation standards. Meeting these requirements protects patient safety, ensures data integrity, and facilitates the smooth progression of a drug candidate through clinical trials to eventual market authorization. Staying aligned with evolving regulatory frameworks is essential for successful drug approval and commercialization.
The Federal Food, Drug, and Cosmetic Act mandates that a sponsor must file an investigational new drug before any clinical study involving a new drug begins in the U.S.
- No early-phase drug = No legal clinical trials.
- Once submitted, the FDA has 30 days to review and issue a “clinical hold” if there are serious concerns.
- If no hold is issued, clinical trials may begin.
3. Ensures Ethical Conduct and Oversight of Human Studies
Ensuring ethical conduct and oversight of human studies is a cornerstone of responsible clinical research. Regulatory bodies, such as the Institutional Review Board (IRB) and ethics committees, review study protocols to guarantee that participant rights, safety, and well-being are prioritized throughout the trial. This oversight ensures that clinical trials comply with ethical guidelines, including informed consent, risk minimization, and confidentiality. Upholding these standards fosters public trust, protects human subjects, and supports the integrity and credibility of the clinical research process.
All experimental drugs must include:
- Institutional Review Board (IRB) approval letters
- Informed Consent Forms (ICFs) for study participants
This protects participant rights by:
- Clearly explaining potential risks and benefits
- Ensuring voluntary participation
- Allowing withdrawal at any time
Sponsors must also include the investigator’s credentials to confirm they are qualified.
4. Ensures Consistent Drug Quality via CMC (Chemistry, Manufacturing & Controls)
The Chemistry, Manufacturing, and Controls (CMC) framework is essential for maintaining consistent drug quality during all stages of pharmaceutical development and production. CMC encompasses the comprehensive analysis and documentation of the drug’s chemical composition, formulation development, manufacturing processes, and quality control measures. This rigorous approach ensures that each batch of the drug product meets strict regulatory standards for purity, potency, stability, and safety. Regulatory agencies like the FDA require detailed CMC data as part of the drug approval process to verify that the manufacturing and quality assurance systems are robust and reproducible. Effective CMC practices guarantee that patients receive medications with reliable therapeutic efficacy and minimal risk.
This section provides details on how the drug is:
- Synthesized
- Formulated
- Packaged and stored
It includes:
- Specifications
- Stability data
- Manufacturing processes
FDA uses this to confirm:
- The drug can be made reproducibly and safely
- The product will remain stable and pure during the study
5. Provides a Scientifically Sound Clinical Plan
The experimental drug must include detailed clinical protocols, describing: Study design (e.g., Phase 1 dose-escalation), Inclusion/exclusion criteria, Safety monitoring plans and Dosing regimens, and endpoints
- FDA reviews the protocol to ensure the trial is:
- Scientifically valid
- Ethically acceptable
- Likely to produce meaningful data
6. Establishes the Foundation for Future Drug Approval

- The new drug is the starting point of the formal drug development process.
- Data from experimental studies feed into:
- New Drug Applications (NDAs) or
- Biologics License Applications (BLAs)
- New drug interactions allow early input from the FDA, helping:
- Optimize clinical trial design
- Avoid regulatory pitfalls
- Streamline future approval
Summary
The new drug is much more than paperwork. It’s a comprehensive safety, ethical, scientific, and legal framework that ensures:
- People are protected
- The drug is of high quality
- Studies are well-designed
- Development proceeds in compliance with U.S. law
Why is the New Drug (Experimental Drug) Critical in Drug Development?
A new drug, often referred to as an experimental drug, is the foundation of pharmaceutical innovation and progress. It represents a novel compound or therapy that is undergoing clinical evaluation to determine its safety, effectiveness, and potential to treat or cure specific medical conditions. The introduction of experimental drugs is critical to advancing healthcare and meeting unmet patient needs.

The new application safeguards human subjects and ensures regulatory oversight. Its approval indicates that:
- Preclinical data support the safety of human trials.
- The manufacturing process is controlled and consistent.
- Investigators are qualified and equipped to conduct human trials.
- The protocol is scientifically valid and ethically approved.
As the foundation for future submissions like NDA (New Drug Application) or BLA (Biologics License Application), the experimental drug/ study drug is a cornerstone of regulatory strategy and clinical development.
Types of New Drug Applications

1. Commercial Study drug:
A Commercial Study Drug refers to a pharmaceutical product that has already received regulatory marketing approval and is being used in a clinical trial for its approved indication. These drugs are often used in post-marketing studies, real-world evidence trials, or comparative effectiveness research to gather additional data on safety, efficacy, or usage patterns in broader patient populations.
Filed by pharmaceutical or biotech companies for eventual drug approval and marketing.
2. Investigator Study drug:
An Investigator Study Drug refers to a pharmaceutical compound used in a clinical trial that is initiated and managed by an independent researcher or clinician, often outside of a commercial sponsor’s direct oversight. These trials are known as Investigator-Initiated Trials (IITs), and the study drug may be a new therapy or an approved drug being tested for a new indication, dosage, or patient population.
Submitted by individual researchers or physicians for studies not intended for commercial use
3. Emergency Study/test drug(EIND)
An emergency study involving a test drug allows for the immediate use of an unapproved therapy in life-threatening or serious conditions when no standard treatment is available and there is not enough time to obtain full regulatory approval. In such cases, the Emergency IND (EIND) process enables clinicians to request rapid FDA authorization to administer the test drug to a single patient or a small group.
Allows the use of an unapproved drug in emergencies without standard review timelines.
4. Treatment Study/test drug
A treatment study is a type of clinical trial designed to evaluate the effectiveness of a new therapy, such as a test drug, in treating a specific disease or medical condition. These studies typically occur during the early to mid-phase of clinical development and are essential for determining the safety, efficacy, and optimal dosing of the test drug in humans.
Permits access to a study drug for patients with serious or life-threatening conditions, even before FDA approval.
FDA Review Process for Early-phase trial application
The FDA review process for early-phase clinical trials—typically Phase I and II—begins with the submission of a clinical trial application, most commonly through an IND submission. This process is designed to ensure patient safety and scientific integrity before a new compound is tested in humans.
- Once submitted, the FDA has 30 calendar days to review the application. During this time:
- No clinical trial may begin unless the experimental drug is not placed on hold.
- If no objection is raised, the test drug becomes “effective”, and human trials can start.
- The FDA may place the test drug on clinical hold if serious concerns arise.
Common Reasons for Early phase drug‘s Clinical Hold
A clinical hold in early phase drug development—typically during Phase I or II trials—can be triggered by various scientific, safety, or regulatory concerns. Understanding these causes is essential for risk mitigation and maintaining trial momentum.
- Inadequate safety data from animal studies
- Poorly designed clinical protocol
- Deficient investigator qualifications
- Incomplete or missing CMC data
- If placed on hold, the sponsor must resolve deficiencies and resubmit the required information.
Maintaining an Active Experimental drug/ Test drug
Maintaining an active experimental drug or test drug throughout clinical trials is crucial for ensuring data integrity, patient safety, and regulatory compliance. Proper handling, storage, and supply chain management help preserve the drug’s stability, potency, and efficacy across all trial phases. Regular quality control checks, real-time monitoring, and seamless logistics ensure that the test drug remains viable from the lab to the patient. Any disruption in availability or quality can delay study timelines, compromise trial outcomes, and impact regulatory approval. By prioritizing the active status of the test drug, sponsors and clinical research teams can safeguard trial success and support a smoother path to market authorization.
- After approval of the experimental drug, sponsors are responsible for:
- Submitting protocol amendments
- Reporting serious adverse events (SAEs)
- Providing annual progress reports
- Maintaining compliance with GCP (Good Clinical Practice) standards
- These ensure ongoing oversight, safety, and scientific integrity of the trials.
Global Equivalents to Study Drug
Though the study drug is specific to the U.S., similar submissions are required worldwide:
| Region | Equivalent to IND |
| EU | IMPD (Investigational Medicinal Product Dossier) |
| Canada | CTA (Clinical Trial Application) |
| India | Clinical Trial Dossier (CTD Format) |
| Japan | Clinical Trial Notification (CTN) |
Conclusion: Why the early-phase drug is the Cornerstone of Clinical Trials
Early phase drug development—especially Phase I and Phase II trials—is the foundation upon which successful clinical research is built. These critical early stages provide essential data on safety, dosage, pharmacokinetics, and initial efficacy, allowing researchers to identify promising candidates and eliminate high-risk compounds early in the pipeline. By reducing late-stage failures, optimizing resource allocation, and accelerating time-to-market, early-phase clinical trials significantly impact the overall success of drug development programs. As the biopharmaceutical industry continues to evolve, investing in robust early phase strategies is no longer optional—it is a strategic imperative. In today’s competitive and highly regulated environment, early phase trials are not just the first step—they are the cornerstone of clinical trial success.
- Understanding and correctly preparing an experimental drug application is a vital regulatory milestone for any pharmaceutical or biotech company. A successful early-phase drug ensures:
- Legal authorization to test in humans
- Early FDA feedback and regulatory alignment
- Streamlined progression to NDA/BLA submissions
- For professionals in regulatory affairs, clinical research, and drug development, mastering the test drug process is not just a requirement; it’s a strategic advantage.
References
- U.S. FDA – New Drug Application
https://www.fda.gov. - FDA Guidance for Industry – Content and Format
https://www.fda.gov/media/72259/download - ICH E6(R2) Guideline for Good Clinical Practice
https://www.ich.org/page/efficacy-guidelines - 21 CFR Part 312 – New Drug Application Regulations
https://www.ecfr.gov/current/title-21/chapter-I/subchapter-D/part-312