Introduction

For decades, the path from laboratory to pharmacy shelf has relied heavily on human trials, large-scale manufacturing plants, and time-consuming regulatory processes. But the pharmaceutical industry is undergoing a seismic shift. A new era is emerging, one where computer-simulated trials predict drug behavior with striking accuracy, and smart, compact micro-factories produce medicines on demand with minimal human intervention.
At the heart of this revolution are two transformative forces: Virtual Bioequivalence (VBE) and AI-driven micro-factories. Virtual Bioequivalence VBE challenges the long-held reliance on clinical testing by offering safe, data-driven alternatives that mimic how drugs perform in the human body, without actually involving humans. Meanwhile, AI-powered manufacturing platforms are redefining production models, transitioning from centralized “mega plants” to agile, localized systems that can produce precision batches in real-time.
This isn’t science fiction. It’s a rapidly unfolding reality, and it’s changing how we develop, test, and deliver medicines. As regulators begin to recognize and validate these technologies, and as pharmaceutical companies race to integrate them, the question is no longer if these innovations will reshape drug development, but how fast.
In this article, we explore how the industry is transitioning “from humans to holograms,” unpack the core science behind virtual bioequivalence, and examine how AI-powered micro-factories are revolutionizing pharmaceutical production from the ground up.
1. The Rise of Virtual Bioequivalence (VBE): When Simulated Trials Replace Human Volunteer Risks
Imagine submitting a full bioequivalence dossier for an Abbreviated New Drug Application (ANDA), without enrolling a single human participant. No early morning fasting visits. No blood draws. No dropouts due to adverse events. Instead, your entire application is backed by predictive computer simulations that emulate how the drug behaves inside a diverse range of virtual human bodies.
Virtual Bioequivalence (VBE) is no longer science fiction. It’s the next frontier of drug development, and it’s unfolding faster than many realize.
The Birth of a New Era in Biopharmaceutics
The traditional approach to bioequivalence (BE) studies, which aims to demonstrate that a generic product behaves similarly to its reference drug, is inherently complex, costly, and ethically taxing. Each study often involves dozens to hundreds of healthy volunteers, extensive blood sampling, and statistical evaluations that must prove pharmacokinetic (PK) metrics like Cmax (maximum plasma concentration) and AUC (area under the curve) fall within an acceptable equivalence window (typically 80–125%).
But what if those PK profiles could be predicted with mathematical precision, using software that accurately simulates drug absorption, distribution, metabolism, and excretion (ADME) in a variety of virtual human models?
The Engine Behind the Revolution: PBPK Modeling
At the core of Virtual Bioequivalence VBE lies Physiologically-Based Pharmacokinetic (PBPK) modeling, a sophisticated computational framework that uses physiological parameters, such as tissue volumes, blood flow rates, enzyme activity levels, and gastrointestinal conditions, to simulate the fate of a drug in the human body.
What sets this apart from traditional pharmacokinetics is its granularity. PBPK doesn’t just track how a drug moves; it models how that movement is influenced by the biology of specific populations, including children, the elderly, patients with liver disease, or individuals with genetic polymorphisms in metabolizing enzymes like CYP3A4.
These models can be tailored with in vitro dissolution data, physicochemical properties (like solubility, logP, permeability), and combined with demographic variability, allowing researchers to simulate virtual trials on entire synthetic populations, spanning multiple ethnicities, genders, body weights, and age ranges.
Where AI and Bayesian Simulation Meet Pharmacokinetics
To handle such complexity, Virtual Bioequivalence VBE frameworks often use Bayesian inference and Monte Carlo simulations, powerful statistical techniques that can simulate variability and uncertainty in clinical data. By generating thousands of virtual subjects, these simulations estimate the likelihood that a test formulation is bioequivalent to a reference with over 90% confidence, in some models.
Artificial intelligence (AI) further enhances the accuracy of these predictions. Machine learning algorithms can train on historical BE outcomes, refine model assumptions, detect patterns that might escape human intuition, and optimize trial design long before the first batch hits the tablet press.
For instance, AI-driven PBPK models can help pinpoint why one formulation might fail due to food effects, or how changes in excipients could delay Tmax (time to reach maximum concentration) in fasted conditions.
Why This Matters, For Everyone Involved?
- Ethical Efficiency: No longer must healthy volunteers face unnecessary exposure to investigational drugs. Virtual Bioequivalence VBE enables drug developers to reduce or, in some cases, eliminate human involvement, especially for drugs with well-characterized pharmacology and low risk.
- Cost and Time Reduction: Traditional BE trials can cost upwards of USD 1 million and take several months. In contrast, a validated Virtual Bioequivalence VBE workflow may take a few weeks and cost a fraction of the price. Plus, trials can be run in parallel for multiple demographics, rather than sequentially.
- Formulation Flexibility. In early development, even small formulation tweaks can require new clinical studies. With Virtual Bioequivalence VBE, formulators can test changes virtually, adjusting particle size, coating polymers, or release kinetics, and seeing how those changes affect absorption profiles. This drastically reduces the cost of iteration.
- Regulatory Momentum Both the FDA and EMA have endorsed model-informed drug development (MIDD) approaches. The FDA’s MIDD pilot program, launched in 2018, has been working with sponsors to accept PBPK models for trial optimization, dose selection, and, yes, bioequivalence justification in certain cases. Similarly, the EMA is working on new guidelines (including the upcoming ICH M13 series) that signal a cautious but forward-looking acceptance of virtual trials, especially for well-characterized generic drugs and complex formulations.
Who’s Already Doing It?
Major pharma and biotech firms have already started to use Virtual Bioequivalence VBE to complement or, in some low-risk situations, replace in vivo studies. A 2023 survey published in Pharmaceutics revealed that nearly 40% of model-based submissions in Europe used PBPK tools to justify or waive certain clinical trial components. Drugs with narrow therapeutic index, pH-dependent solubility, or colonic release targets are increasingly seen as strong candidates for Virtual Bioequivalence VBE.
One such example involves a PBPK model for acyclovir, which simulated food effects on absorption. The results were later verified in a small clinical study and found to be in near-perfect alignment, paving the way for future BE waivers in similar formulations.
Challenges on the Horizon
Despite the optimism, Virtual Bioequivalence VBE is not a universal solution, at least not yet.
- Model credibility remains a sticking point. Regulators demand complete transparency about model structure, input data, and assumptions.
- Validation requirements are steep: developers must show that the model accurately reproduces observed clinical data for the same API.
- Black-box AI is discouraged. Regulators prefer explainable, auditable systems, not opaque algorithms.
Still, the writing is on the wall. As computational power grows and regulatory science evolves, the industry is inching toward a paradigm where human trials are no longer the bottleneck in development.
Humanizing the Shift
Perhaps the most remarkable aspect of Virtual Bioequivalence VBE isn’t the technology; it’s what it means for people. It means fewer risks for healthy volunteers. It means faster access to affordable medicine for patients who can’t wait. It means small-scale pharmaceutical innovators can compete with big players by making smart, model-driven decisions early on. It means regulators, scientists, and patients are all working from the same, transparent digital blueprint.
2. How Virtual Bioequivalence Works: A Blend of Science, Data & Population Modeling
Gone are the days when bioequivalence (BE) assessments were strictly tethered to a clinic, a cohort of healthy volunteers, and a long queue of plasma samples. Today, the science of pharmacokinetics is being reimagined inside supercomputers, where the human body is not just modeled, but meticulously simulated down to the enzymatic and molecular level. This isn’t about replacing clinical trials entirely, at least not yet. It’s about empowering scientists with predictive tools that are fast, cost-effective, and scientifically robust.
Step 1: Gathering Mechanistic and Physicochemical Data
Every virtual bioequivalence (VBE) simulation starts with a solid empirical foundation. Scientists begin by collecting a rich dataset describing the drug’s behavior in vitro and its physicochemical traits. This includes:
- Dissolution profiles across pH conditions (acidic stomach, neutral intestine, etc.)
- Solubility, permeability, pKa, logP, and particle size distribution
- Formulation characteristics like granule morphology, coating thickness, and release kinetics
These inputs are not trivial; any error in this data can lead to flawed simulations and failed regulatory submissions. Hence, the phrase “garbage in, garbage out” couldn’t be more relevant here.
Step 2: Building the PBPK Model – A Virtual Human in Code
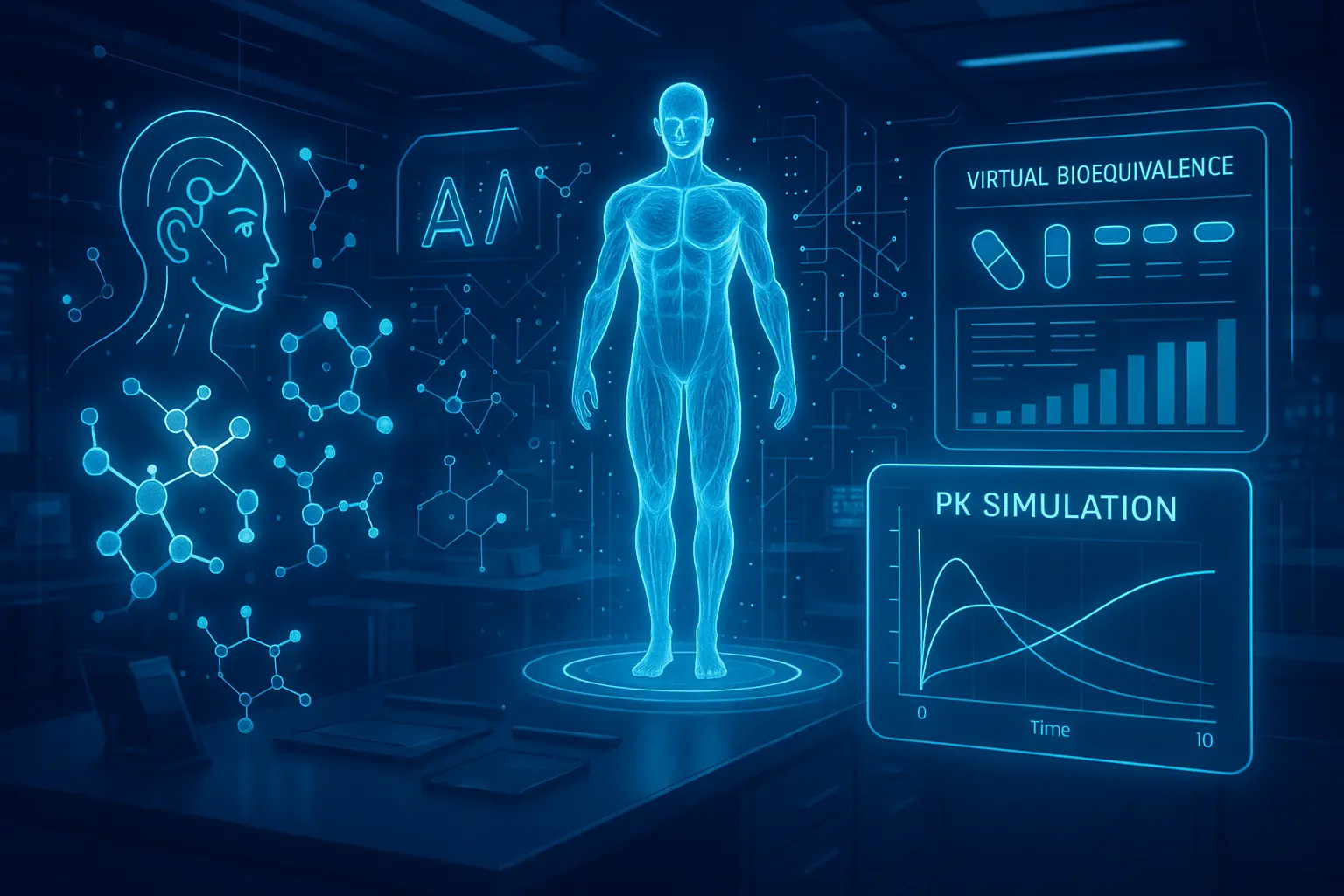
Once the drug’s characteristics are mapped, the next step is constructing a Physiologically-Based Pharmacokinetic (PBPK) model. Think of this model as a digital twin of a human being. It simulates how the drug travels through the body: from the moment it’s swallowed or injected, through the bloodstream, into the liver for metabolism, and eventually out via the kidneys or feces. The model integrates:
- Anatomical data (organ sizes, blood flow)
- Biochemical parameters (enzyme expression, transporter activity)
- Demographic variables (age, sex, weight, ethnicity)
- Pathophysiological factors (hepatic impairment, renal dysfunction, pregnancy, etc.)
Platforms like Simcyp, PK-Sim, and GastroPlus help researchers run simulations tailored to specific populations, such as elderly patients, neonates, or those with compromised metabolism.
Step 3: Simulating Population Variability
No two individuals respond to a drug in the same way. That’s where statistical modeling steps in, particularly Bayesian inference and Monte Carlo simulations. These tools generate thousands of virtual subjects, each with slightly different physiological and biochemical parameters. The simulations assess inter-subject variability (differences between people) and intra-subject variability (differences in the same person across days or meals), capturing the natural complexity of real-world pharmacokinetics.
- A Monte Carlo simulation might model 10,000 virtual patients taking both the test and reference formulations.
- The outcome? A full distribution of PK metrics like Cmax, AUC, and Tmax, ready for statistical evaluation.
Step 4: Running the Virtual Bioequivalence Trial
With all the pieces in place, scientists now run side-by-side digital comparisons of the test formulation (generic) and the reference product (usually the brand-name innovator). The software calculates:
- Cmax – peak plasma concentration
- AUC – area under the plasma concentration-time curve
- Tmax – time to reach peak concentration
Regulatory guidelines (from FDA and EMA) require that the 90% confidence intervals for the test/reference ratios of Cmax and AUC fall within the 80–125% bioequivalence window. In a virtual study, this is translated into probabilistic terms:
- For example, “93% of simulated subjects fell within the BE window” may be considered acceptable.
These simulations can be completed in a matter of days, long before clinical recruitment or lab analysis would even begin.
Step 5: Regulatory Scrutiny and Model Credibility
Though the science is solid, regulators are careful. Agencies like the FDA and EMA are opening their doors to VBE but with strict caveats:
- Models must be fully transparent; no “black-box” AI allowed
- All assumptions and inputs must be justified and traceable
- Models should be validated against real clinical data
- Full audit trails and version control are mandatory
Under the FDA’s Model-Informed Drug Development (MIDD) initiative, numerous sponsors have already engaged in pilot programs to gain partial or full waivers from traditional BE studies. The EMA’s evolving ICH M13 guideline series further reinforces the legitimacy of these in silico approaches, especially for modified-release drugs and generics with well-understood mechanisms.
Why It Matters?
This isn’t just a technical revolution, it’s a moral and practical one. Virtual bioequivalence protects human volunteers from unnecessary exposure. It gives smaller pharma companies access to high-quality development without the budget of Big Pharma. And it drastically accelerates access to affordable generics and personalized formulations, especially in regions where clinical trial infrastructure is limited.
Conclusion: From Data Points to Decisions, A Revolution Without a Pulse
We stand at the brink of a pharmaceutical renaissance, one where clinical trials no longer begin with a call for volunteers, but with a line of code. Virtual Bioequivalence (vBE) and Model-Informed Bioequivalence (MIBE) are not mere innovations; they are instruments of liberation: freeing patients from unnecessary exposure, freeing companies from regulatory inertia, and freeing science from outdated traditions that no longer serve progress.
In this paradigm, models don’t just simulate, they anticipate. They don’t just mimic, they evolve. And perhaps most importantly, they don’t aim to replace human judgment but to amplify it. The human formulator is no longer confined to the slow loop of trial and error but empowered to explore, adapt, and optimize with unprecedented precision. What once took quarters can now happen in weeks, sometimes days, with higher confidence, lower cost, and vastly greater ethical clarity.
Regulators are no longer gatekeepers; they’re partners in innovation. The question is no longer “Can we skip the trial?” It’s “Do we understand the science deeply enough to not need one?”
As we move from humans to holograms, from clinics to code, and from pills to pixels, one thing is certain: we are not just digitizing drug development, we are humanizing it. We are creating a world where patients benefit sooner, scientists build smarter, and innovation walks hand-in-hand with responsibility.
So yes, the trials of the future may be silent. No footsteps down a clinic corridor. No vials of blood. No handwritten forms. But make no mistake, the impact will echo louder than ever.
Welcome to the age where science thinks, and medicine moves at the speed of trust.
References
- Shebley, M., et al. (2020). “Physiologically Based Pharmacokinetic (PBPK) Modeling and Simulation for Regulatory Applications: Prospective Decision Making and Labeling.” Clinical Pharmacology & Therapeutics, 107(3), 654–664.
- Alotaiq, N., & Dermawan, J. (2024). “Advancements in Virtual Bioequivalence Modeling for Regulatory Decision-Making.” Pharmaceutics, 16(2), 240.
- FDA. (2022). “Model-Informed Drug Development (MIDD) Paired Meeting Pilot Program.” https://www.fda.gov
- EMA. (2024). “ICH M13A Guideline on Bioequivalence for Immediate-Release Orally Administered Drug Products.” https://www.ema.europa.eu
- Zhao, P., et al. (2011). “Applications of PBPK Modeling and Simulation during Regulatory Review.” Clinical Pharmacology & Therapeutics, 89(2), 259–267.
- Polak, S., & Rostami-Hodjegan, A. (2020). “Virtual Trials for Predicting Bioequivalence: Is There a Path to Approval?” Frontiers in Pharmacology, 11, 538.
- Kesisoglou, F., et al. (2019). “The Role of In Silico Modeling in Optimizing Product Development.” AAPS Journal, 21(5), 95.
- Alotaiq, A., & Dermawan, R. (2024). Virtual Bioequivalence: Correlating In Silico with In Vivo Outcomes. Pharmaceutics.
- FDA. (2023). Model-Informed Drug Development Pilot Program – www.fda.gov
- EMA. (2022). Reflection Paper on the Use of PBPK Modeling in Generic Applications – www.ema.europa.eu
- Polak, S. et al. (2021). PBPK Models in Regulatory Submissions: A European Perspective. Journal of Pharmacokinetics and Pharmacodynamics.
- Jamei, M. et al. (2020). Simcyp Simulator: Applications in Drug Development. The AAPS Journal.