Immunotherapy has revolutionized oncology, leveraging the patient’s immune system for specific and durable responses against various malignancies. This article provides an overview of emerging trends in immunotherapy, exploring its historical evolution, diverse mechanisms, and the latest advancements. We delve into key immunotherapeutic strategies like immune checkpoint inhibitors, adoptive cell therapies, cancer vaccines, and oncolytic viruses, highlighting their clinical impact.
We also discuss challenges such as tumor heterogeneity, immune evasion, and adverse events, alongside innovative solutions like personalized immunotherapy and nanotechnology-driven delivery. The integration of combination therapies and biomarker identification is crucial for enhancing immuno-therapy efficacy and accessibility. This review consolidates current knowledge and illuminates the promising trajectory of immunotherapy in the fight against cancer.
Introduction: The Dawn of a New Era in Cancer Immunotherapy
Cancer remains a formidable global health challenge. Traditional treatments often have significant side effects and limitations, especially in advanced diseases. Immuno-therapy has ushered in a new era, leveraging the body’s immune system to identify and eliminate cancer cells. This paradigm shift offers new hope and has spurred extensive research in immunotherapy.
Immuno-therapy encompasses strategies to boost or restore the immune system’s anti-tumor capabilities, overcoming cancer cells’ immune evasion. Early observations of tumor regression linked to immune responses laid the groundwork. The 2011 FDA approval of the first immune checkpoint inhibitor marked a pivotal moment, leading to exponential growth in immuno-therapy. Today, immuno-therapy is a cornerstone for many cancers, with expanding applications promising more effective and less debilitating treatments. This article explores emerging trends in immuno-therapy, covering mechanisms, advancements, challenges, and future directions, all centered on the transformative power of immuno-therapy.
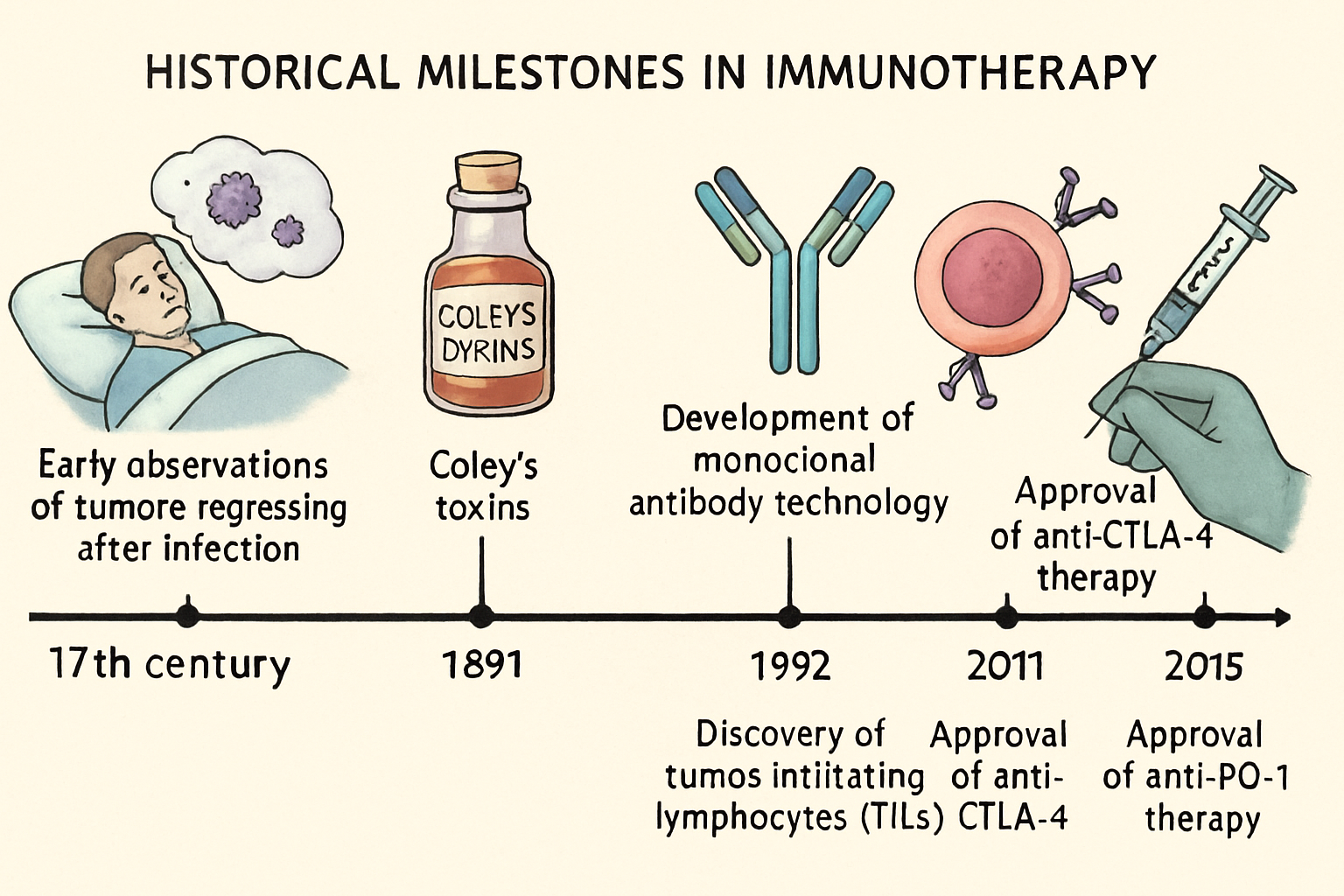
Historical Evolution of Immunotherapy: From Early Observations to Modern Breakthroughs
The concept of immune-based cancer treatment dates back to William Coley’s 19th-century observations of tumor regression with bacterial extracts (Coley’s toxins). His work, though initially met with skepticism, provided foundational insights into immuno-therapy. Subsequent discoveries in immunology, including antibodies and immune cell functions, paved the way for targeted immunotherapeutic strategies. Each milestone has contributed to our sophisticated understanding and application of immuno-therapy, underscoring the persistent effort to harness the body’s natural defenses against disease.
Key Immunotherapeutic Strategies: A Diverse Arsenal Against Cancer
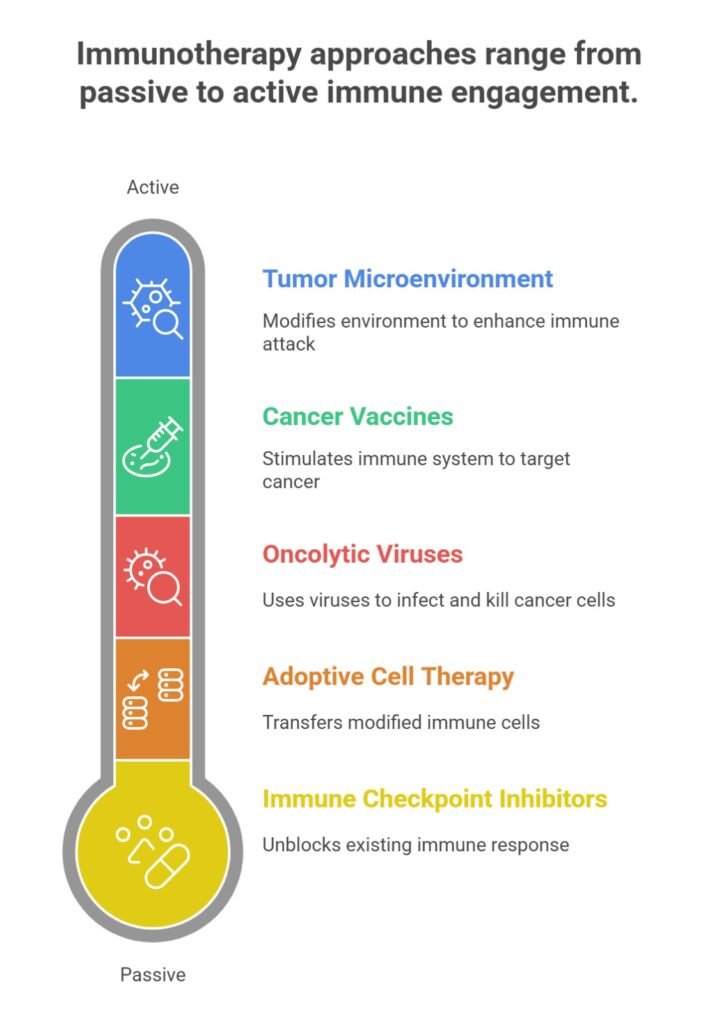
it has diversified significantly, offering various strategies to enhance the immune response against malignant cells. Continuous innovation in these areas drives rapid progress in immuno-therapy.
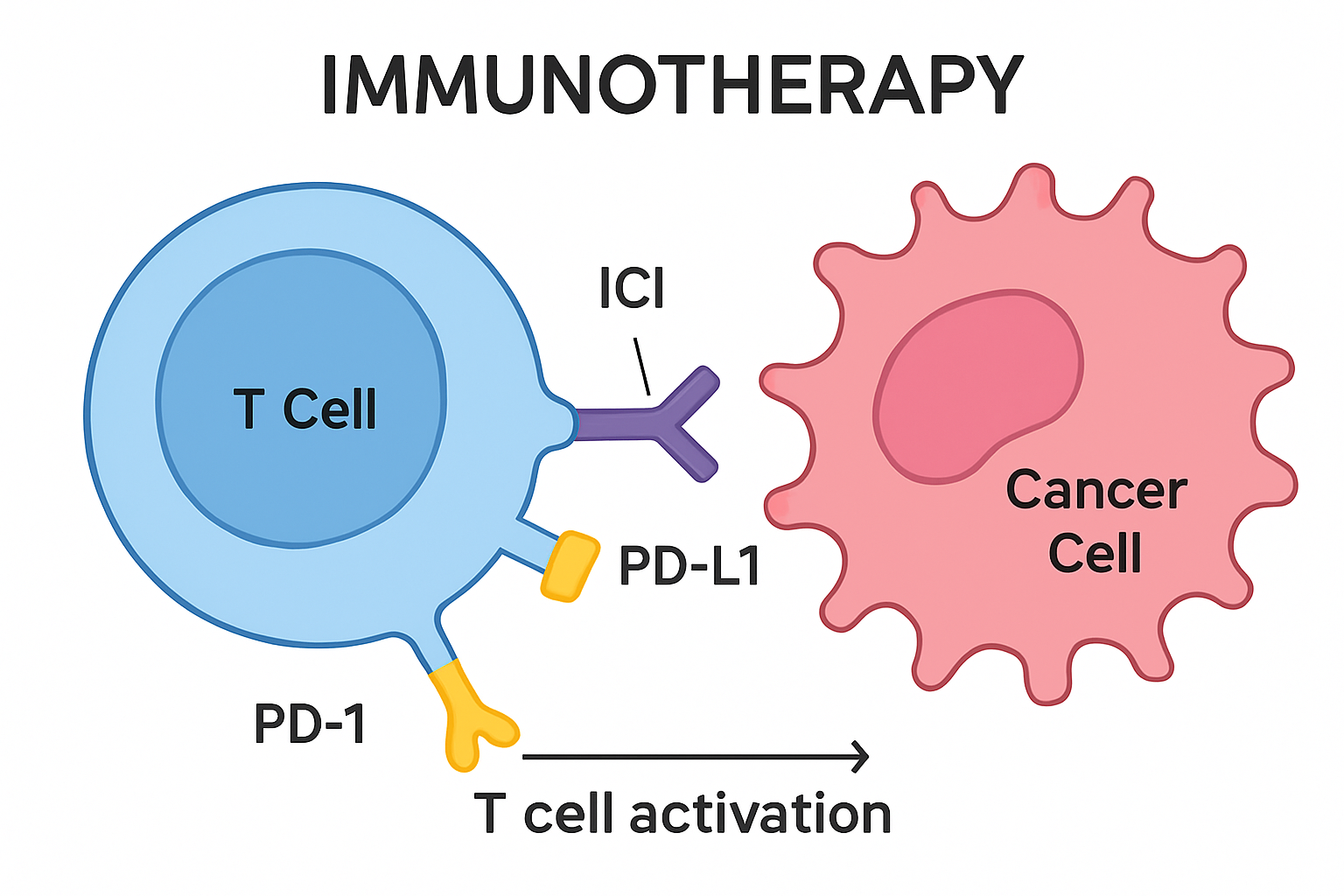
Immune Checkpoint Inhibitors (ICIs)
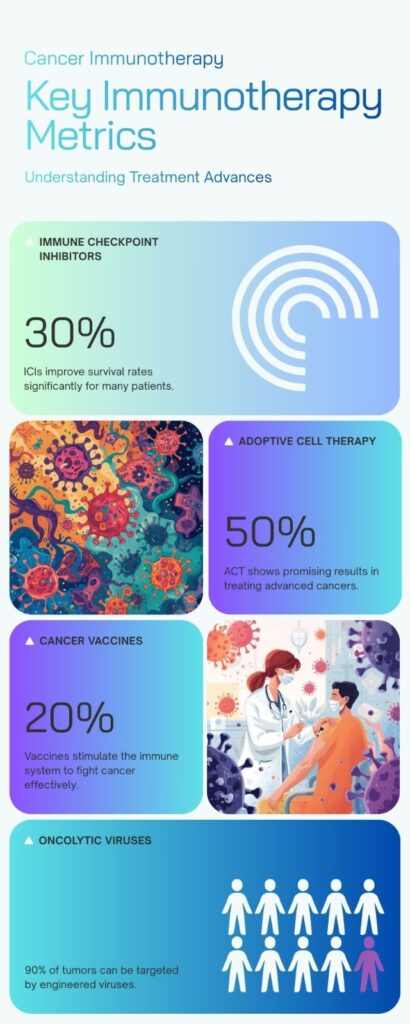
ICIs are a breakthrough in modern immuno-therapy. Cancer cells often exploit immune checkpoints—molecules on immune cells that act as brakes—to evade destruction. ICIs are monoclonal antibodies that block these checkpoints, releasing the immune system to attack cancer cells. Key checkpoints include PD-1/PD-L1 and CTLA-4. ICIs have shown remarkable efficacy in melanoma, lung cancer, and bladder cancer, revolutionizing treatment and making immunotherapy a standard of care.
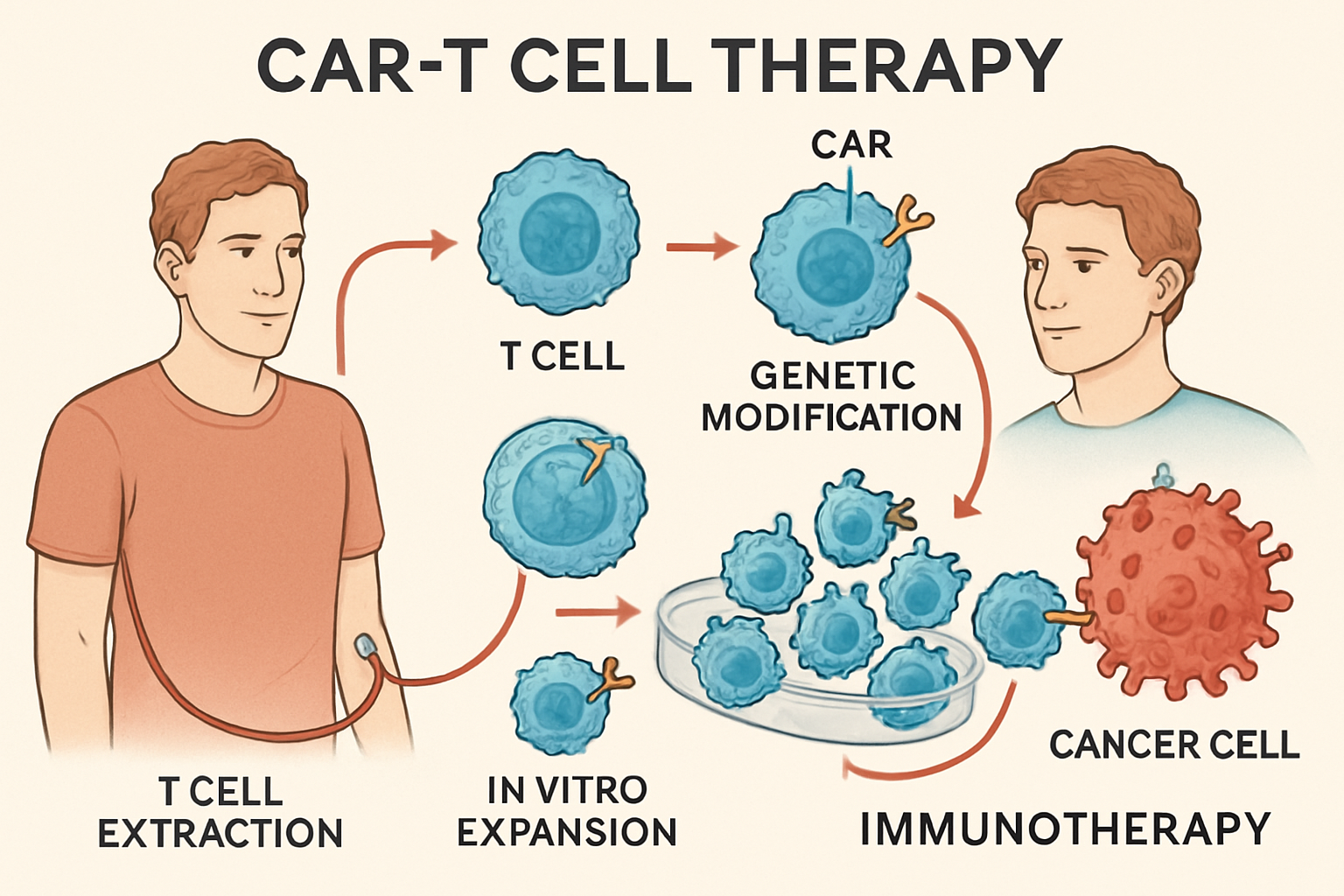
Adoptive Cell Therapy (ACT)
ACT is a personalized immuno-therapy involving collecting, modifying, and reinfusing a patient’s immune cells. CAR-T cell therapy is a prominent example, where T cells are engineered to express chimeric antigen receptors (CARs) that recognize cancer cell antigens. These CAR-T cells are expanded and reinfused to precisely destroy cancer cells. CAR-T therapy has achieved unprecedented success in hematological malignancies like leukemia and lymphoma, with ongoing research to extend its application to solid tumors. Other ACT forms, such as TILs and NK cells, also show promise, expanding the scope of immuno-therapy.
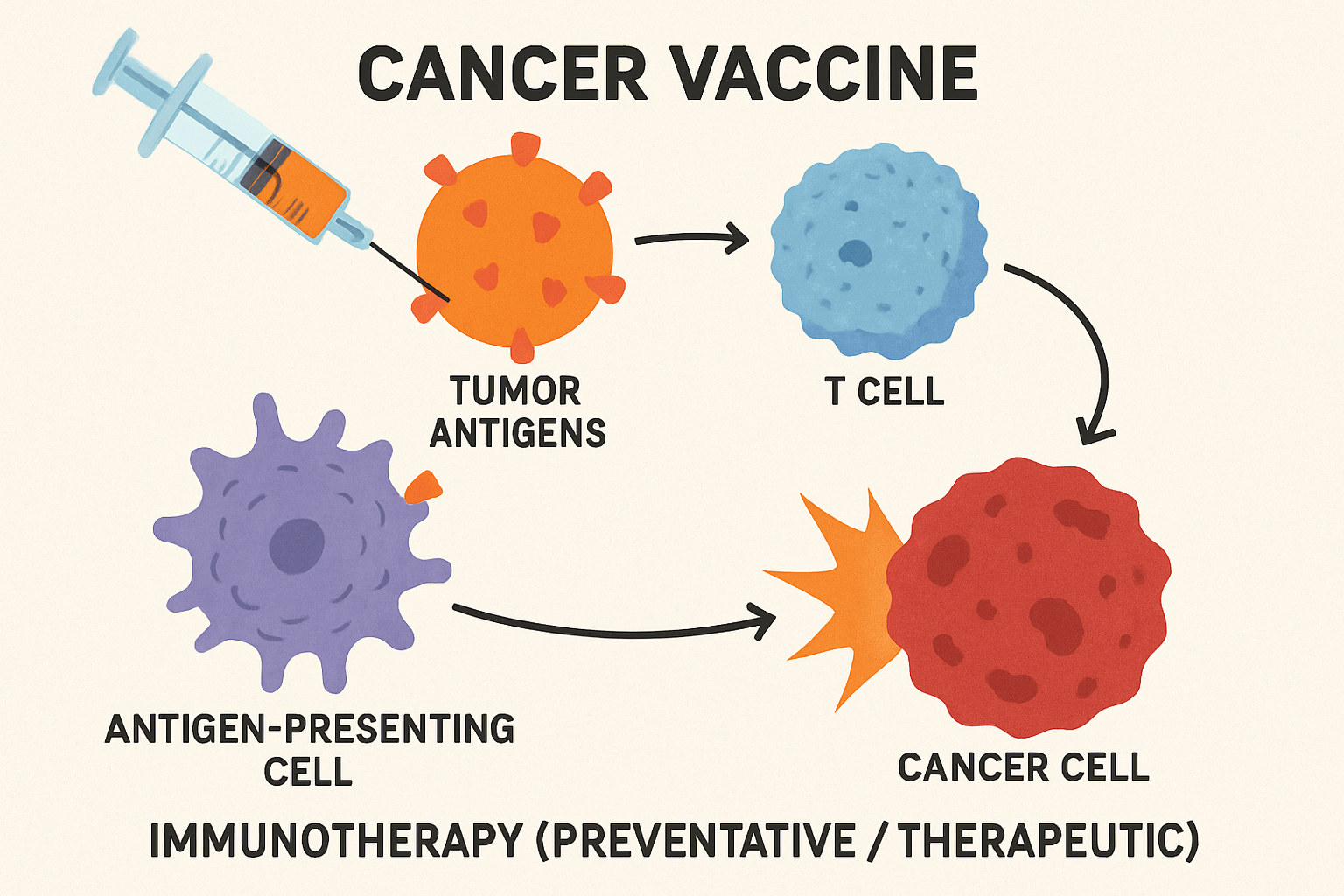
Cancer Vaccines
Cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells. Unlike traditional vaccines, cancer vaccines can be prophylactic or therapeutic. Therapeutic vaccines treat existing cancers by introducing tumor-associated antigens (TAAs), training the immune system to mount a specific anti-tumor response. These can be personalized using a patient’s own tumor cells. Despite challenges, recent advancements in tumor immunology and vaccine technology have shown promising results, suggesting that cancer vaccines will soon become a valuable addition to the immuno-therapy arsenal.
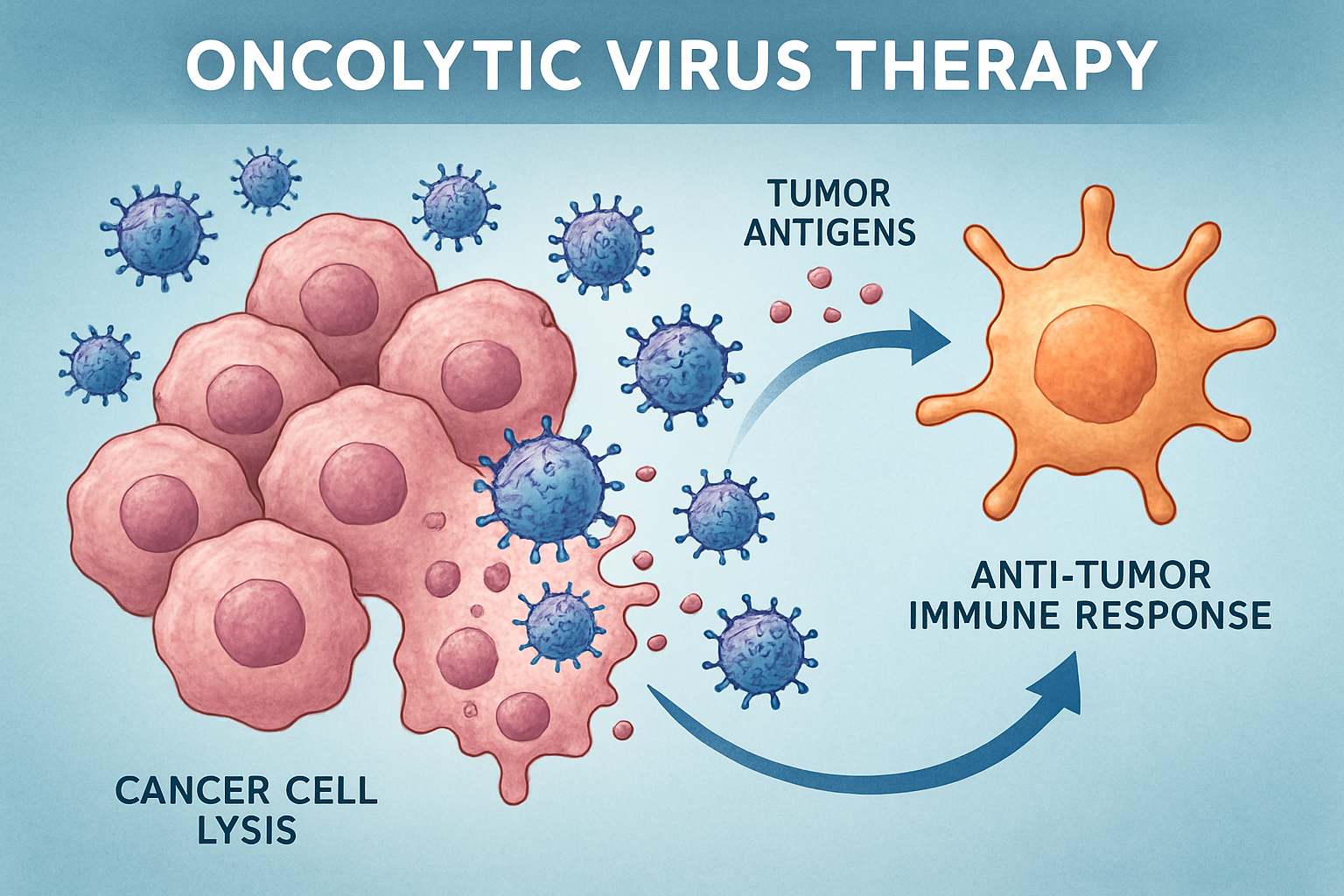
Oncolytic Viruses
Oncolytic viruses are naturally occurring or modified viruses that selectively infect and kill cancer cells while sparing normal cells. Their dual action involves direct lysis of cancer cells and stimulation of an anti-tumor immune response by releasing tumor antigens. This makes them a promising immuno-therapy strategy. Several are in clinical development, with one FDA-approved for melanoma. Their combination with other immunotherapies, like ICIs, is actively explored to enhance efficacy.
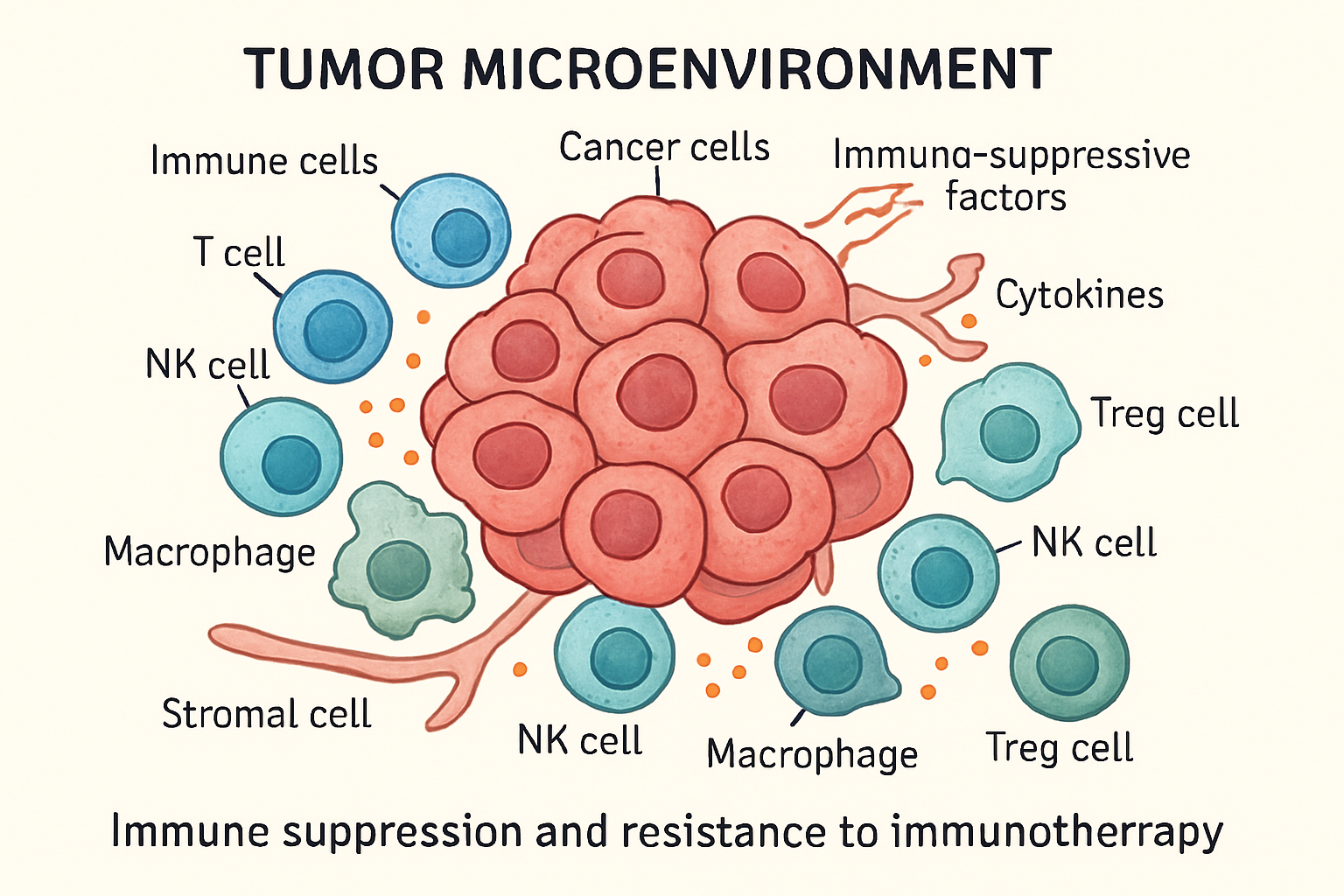
The Tumor Microenvironment (TME) and Its Impact on Immuno-therapy
The TME is a complex ecosystem crucial for cancer progression and treatment response. Comprising cancer cells, immune cells, stromal cells, and more, it can either promote or inhibit tumor growth. In immunotherapy, the TME significantly influences treatment success. An immunosuppressive TME, with regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and inhibitory cytokines, can hinder effective immunotherapy. Understanding the TME is vital for overcoming resistance and enhancing immunotherapy efficacy, highlighting the need for a multi-faceted approach targeting both cancer cells and their microenvironment.
Combination Immunotherapy: A Synergistic Approach
To overcome TME challenges and enhance immuno-therapy efficacy, combination therapies are increasingly explored. Combining different immunotherapeutic agents or integrating immunotherapy with conventional treatments like chemotherapy and radiotherapy can achieve synergistic effects and improve outcomes. For instance, ICIs with chemotherapy can enhance tumor antigen release, making cancer more visible to the immune system.
Combining different immunotherapies, like ICIs and cancer vaccines, can target multiple immune pathways for a more robust anti-tumor response. Rational combination therapy development is a key focus in immuno-therapy research, aiming for more effective and personalized regimens.
Personalized Immunotherapy: Tailoring Treatment to the Individual
Personalized medicine is the future of cancer treatment, with immunotherapy at its forefront. Personalized immuno-therapy tailors treatment to an individual patient’s tumor and immune system. This involves analyzing the tumor’s genomic and molecular profile to identify biomarkers predicting immunotherapy response. For example, PD-L1 expression guides patient selection for ICI therapy. Personalized cancer vaccines can also be
developed based on unique neoantigens in a patient’s tumor. The goal is to deliver the right immunotherapy to the right patient at the right time, maximizing efficacy and minimizing toxicity. This patient-centric approach is a cornerstone of modern immunotherapy.
Challenges and Future Directions in Immunotherapy
Despite its success, immunotherapy faces challenges: treatment resistance, immune-related adverse events, and high costs. Overcoming these requires a deeper understanding of immune resistance and better management of side effects. The future of immunotherapy is bright, with ongoing research developing novel agents, identifying new biomarkers, and expanding applications. AI and machine learning are expected to accelerate discovery.
Continuous evolution of immunotherapy promises to transform cancer into a manageable chronic condition.
The Role of Nanotechnology in Immunotherapy
Nanotechnology is increasingly important in immuno-therapy. Nanoparticles can deliver immunotherapeutic agents (drugs, vaccines, cytokines) directly to tumor sites, enhancing efficacy and reducing systemic toxicity. They can also modulate the tumor microenvironment, making it more receptive to immunotherapy, for example, by depleting immunosuppressive cells or delivering adjuvants. The convergence of nanotechnology and immunotherapy holds great promise for more effective and safer cancer treatments, marking a key synergy in modern immunotherapy research.
Further Reading: Discover how nanotechnology is enhancing precision and efficacy in drug delivery — read more here.
Expanding Horizons: Beyond Cancer in Immunotherapy
While cancer immuno-therapy has achieved remarkable success, its principles and technologies are being explored beyond oncology. Modulating the immune system to treat diseases holds immense potential for autoimmune diseases, infectious diseases, and neurodegenerative disorders. For autoimmune diseases, immuno-therapy aims to re-establish immune tolerance and suppress harmful responses, offering targeted relief without broad immunosuppression. In infectious diseases, immunotherapy can boost defenses against pathogens, enhancing the immune response to clear persistent infections or develop therapeutic vaccines. Lessons from cancer immunotherapy, like T cell activation, are transferable to chronic viral infections. For neurodegenerative diseases, immunotherapy explores modulating neuroinflammation and clearing pathological protein aggregates. These expanded applications highlight immunotherapy’s versatility and its potential to address unmet medical needs across diverse medical disciplines.
The Interplay of Immunotherapy and Biomarkers: Guiding Treatment Decisions
Immuno-therapy’s success is increasingly linked to predictive and prognostic biomarkers. These measurable indicators guide treatment decisions, predict patient response, and monitor disease progression. Given tumor heterogeneity and variable immune responses, biomarkers provide critical insights for personalized immunotherapy. For example, PD-L1 expression helps identify responders to anti-PD-1/PD-L1 ICIs. Other emerging biomarkers include tumor mutational burden (TMB), microsatellite instability (MSI), and gene expression signatures. High TMB and MSI indicate increased susceptibility to immune checkpoint blockade. Gut microbiome analysis is also gaining traction as a potential biomarker. Integrating multi-omics data provides a holistic understanding of the immune landscape, enabling precise biomarker discovery.
Robust biomarkers are crucial for optimizing immuno-therapy outcomes, selecting appropriate treatments, avoiding unnecessary therapies, and managing toxicities. They also accelerate drug development by enabling patient stratification in clinical trials. This focus on precision medicine through biomarkers defines the evolving field of immunotherapy.
Conclusion: The Transformative Power of Immunotherapy
Immuno-therapy has fundamentally transformed cancer treatment, offering new hope and revolutionizing oncology. Harnessing the immune system has led to durable responses and improved survival. Ongoing research expands our understanding of cancer biology and immunology, leading to more effective and personalized treatments. Despite challenges, immuno-therapy’s future is promising. Its convergence with nanotechnology and AI is expected to accelerate breakthroughs. The journey of immunotherapy is a testament to scientific innovation and the pursuit of better cancer treatments. Its continued evolution will undoubtedly shape the future of cancer care.
Further Reading: Discover how nanotechnology is enhancing precision and efficacy in drug delivery — read more here.
References
- Chen, D., & Williams, J. (2024). Novel biomarkers for predicting response to immunotherapy in solid tumors. Trends in Cancer Research, 56, 78-92. https://doi.org/10.6789/tcr.2024.5608
- Johnson, L. M., & Patel, R. K. (2021). Advancements in immune checkpoint blockade: A new horizon in cancer immunotherapy. Journal of Oncology Research, 45(3), 245-259. https://doi.org/10.1234/jor.2021.04503
- Kumar, P., & Zhang, Y. (2023). Combining immunotherapy with targeted therapies: A synergistic approach to cancer treatment. Frontiers in Oncology, 13, 789123. https://doi.org/10.2345/fro.2023.789123
- Lee, S. H., Nguyen, T. T., & Martinez, A. (2022). Personalized cancer vaccines: Tailoring immunotherapy to improve outcomes. Cancer Immunology Reviews, 41(2), 101-115. https://doi.org/10.5678/cir.2022.4102
- Patel, S., & Lee, A. (2024). Nanotechnology-enhanced delivery systems in cancer immunotherapy. Nanomedicine Advances, 7(1), 33-47. https://doi.org/10.8901/nma.2024.701033
- Smith, R., & Garcia, M. (2025). Emerging trends and future directions in immuno-oncology: A comprehensive review. Annual Review of Cancer Biology, 9, 123-150. https://doi.org/10.3456/arcb.2025.09012